Avecin-N solution for infusion 400 mg/250 ml bottle 250 ml No. 1

Instructions Avecin-N solution for infusion 400 mg/250 ml bottle 250 ml No. 1
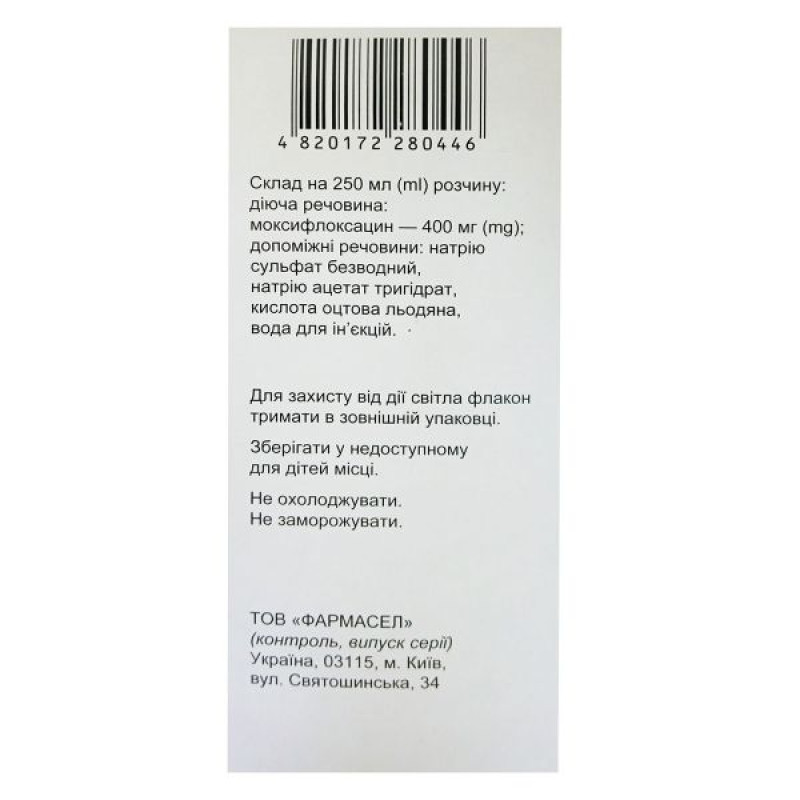
Composition
active ingredient moxifloxacin;
1 bottle (250 ml) contains 400 mg of moxifloxacin, equivalent to 436 mg of moxifloxacin hydrochloride;
excipients sodium sulfate anhydrous, sodium acetate trihydrate, glacial acetic acid (for pH adjustment), water for injections
Dosage form
Solution for infusion
Main physicochemical properties: clear yellow solution without visible particles
Pharmacotherapeutic group
Antimicrobial agents for systemic use Antibacterial agents of the quinolone group ATX code J01M A14
Pharmacological properties
Pharmacodynamics.
Mechanism of action
Moxifloxacin inhibits bacterial type II topoisomerases (DNA gyrase and topoisomerase IV), which are essential for bacterial DNA replication, transcription and repair. Pharmacokinetics/pharmacodynamics
The ability of fluoroquinolones to kill bacteria directly depends on their concentration. Pharmacodynamic studies of fluoroquinolones in animal models of infectious and inflammatory diseases and in humans indicate that the main determinant of efficacy is the ratio between the area under the pharmacokinetic curve (AUC24) and the minimum inhibitory concentration (MIC)
Mechanism of resistance
Resistance to fluoroquinolones can arise from mutations in DNA gyrase and topoisomerase IV. Other mechanisms include overexpression of efflux pumps, impermeability, and protein-mediated protection of DNA gyrase.
Cross-resistance may be expected between moxifloxacin and other fluoroquinolones. Resistance mechanisms common to antibacterial agents belonging to other classes do not affect the antibacterial efficacy of moxifloxacin.
Limit values
Clinical MICs and disk diffusion test breakpoints for moxifloxacin as determined by EUCAST (European Committee on Antimicrobial Susceptibility Testing) (01 01 2012)
| Microorganism | Sensitive | Resistant |
| Staphylococcus spp. | ≤ 0.5 mg/l ³ 24 mm | > 1 mg/l 21 mm |
| Streptococcus pneumoniae | ≤ 0.5 mg/l ³ 22 mm | > 0.5 mg/l 22 mm |
| Streptococcus groups A, B, C, G | ≤ 0.5 mg/l ³ 18 mm | > 1 mg/l 15 mm |
| Haemophilus influenzae | ≤ 0.5 mg/l ³ 25 mm | > 0.5 mg/l 25 mm |
| Moraxella catarrhalis | ≤ 0.5 mg/l ³ 23 mm | > 0.5 mg/l 23 mm |
| Enterobacteriaceae | ≤ 0.5 mg/l ³ 20 mm | > 1 mg/l 17 mm |
| Limit values not related to the bacterial species* | ≤ 0.5 mg/l | > 1 mg/l |
| *Non-species breakpoints were determined primarily based on the relationship between pharmacokinetic and pharmacodynamic data and are independent of MICs for individual species. These data are used for species that do not have individually defined breakpoints and are not used for species where interpretive criteria are to be determined. |
Microbiological susceptibility
The prevalence of acquired resistance of isolated species may vary with location and time, therefore local information on resistance is necessary, especially when treating severe infections. Specialist advice should be sought when the local prevalence of resistance is such that the benefit of the medicinal product, at least for some types of infections, is questionable.
| Typically susceptible species of microorganisms |
Aerobic Gram-positive microorganisms Staphylococcus aureus*+ Streptococcus agalactiae (group B) Streptococcus milleri group* (S anginosus, S constellatus and S intermedius) Streptococcus pneumoniae* Streptococcus pyogenes* (group A) Streptococcus viridans group (S viridans, S mutans, S mitis, S sanguinis, S salivarius, S thermophilus) |
Aerobic Gram-negative microorganisms Acinetobacter baumanii Haemophilus influenzae* Legionella pneumophila Moraxella (Branhamella) catarrhalis* |
Anaerobic microorganisms Prevotella spp. |
Other microorganisms Chlamydophila (Chlamydia) pneumoniae* Coxiella burnetii Mycoplasma pneumoniae* |
| Species in which resistance may develop |
Aerobic Gram-positive microorganisms Enterococcus faecalis* Enterococcus faecium* |
Aerobic Gram-negative microorganisms Enterobacter cloacae* Escherichia coli*# Klebsiella pneumoniae*# Klebsiella oxytoca Proteus mirabilis* |
Anaerobic microorganisms Bacteroides fragilis* |
| Resistant microorganisms |
Aerobic Gram-negative microorganisms Pseudomonas aeruginosa |
*Effectiveness sufficiently demonstrated in clinical studies +Methicillin-resistant Staphylococcus aureus is very often simultaneously resistant to fluoroquinolones. In methicillin-resistant Staphylococcus aureus, the level of resistance to moxifloxacin is over 50%. #Strains that produce extended-spectrum β-lactamase (ESBL) are also resistant to fluoroquinolones |
Pharmacokinetics.
After a single infusion of 400 mg moxifloxacin over 1 hour, the maximum concentration (Cmax) is reached at the end of the infusion and is approximately 4.1 mg/l, which is approximately 26% higher than that after oral administration of moxifloxacin (3.1 mg/l). The AUC is approximately 39 mg×h/l after intravenous administration, which is only slightly higher than that after oral administration of moxifloxacin (35 mg×h/l); the absolute bioavailability is approximately 91%. When moxifloxacin is administered intravenously, there is no need for dose adjustment according to the age or gender of the patients. The pharmacokinetics are linear in the range of 50–200 mg for a single oral dose, up to 600 mg for a single intravenous dose and up to 600 mg for once daily administration for 10 days.
Distribution
Moxifloxacin is rapidly distributed in the extravascular space. The volume of distribution at steady state (Vss) is approximately 2 l/kg. In vitro and ex vivo studies have shown that protein binding is approximately 40-42%, independent of concentration. Moxifloxacin is mainly bound to serum albumin. Peak concentrations of 5.4 mg/kg and 20.7 mg/l (geometric mean) were observed in bronchial mucosa and epithelial lining fluid, respectively, 2.2 hours after oral dosing. The corresponding peak concentration in alveolar macrophages was 56.7 mg/kg. In cutaneous vesicle fluid, a concentration of 1.75 mg/l was observed 10 hours after intravenous administration. The free concentration-time profile for interstitial fluid is similar to that for plasma, with a maximum free concentration of 1.0 mg/l (geometric mean) achieved approximately 1.2 hours after oral dosing. 1.8 hours after intravenous administration of moxifloxacin
Metabolism
Moxifloxacin undergoes phase II biotransformation and is excreted from the body by the kidneys (approximately 40%) and with feces/bile (approximately 60%) both in an unchanged form and in the form of sulfoconjugates (M1) and glucuronides (M2). M1 and M2 are metabolites relevant only for humans, both of which are microbiologically inactive. No metabolic pharmacokinetic interactions with other drugs involved in phase I biotransformation, including cytochrome P450 enzymes, were observed in in vitro studies and phase I clinical studies. No evidence of oxidative metabolism
Breeding
The plasma half-life of moxifloxacin is approximately 12 hours. The mean estimated total clearance after administration of 400 mg is 179 to 246 ml/min. After intravenous administration of 400 mg, the excretion of moxifloxacin in urine as unchanged drug was approximately 22% and in feces - 26%. The total excretion of the dose (unchanged moxifloxacin and metabolites) was approximately 98% after intravenous administration of the drug. Renal clearance is approximately 24-53 ml/min, indicating partial tubular reabsorption of the drug from the kidneys. Concomitant administration of ranitidine and probenecid with moxifloxacin does not change the renal clearance of the drug.
Kidney failure
No significant changes in the pharmacokinetics of moxifloxacin were found in patients with impaired renal function (including patients with creatinine clearance > 20 ml / min / 1.73 m2). With a decrease in renal function, the concentration of metabolite M2 (glucuronide) increases almost 2.5 times (with creatinine clearance 2)
Liver dysfunction
Data from pharmacokinetic studies conducted in patients with hepatic insufficiency (Child-Pugh class A, B) do not allow definitively determining whether there are any differences in the parameters of patients with impaired hepatic function and healthy volunteers. Impaired hepatic function was associated with higher plasma exposure to M1, while the exposure to the parent drug was similar to that in healthy volunteers. There is insufficient clinical experience with moxifloxacin in patients with impaired hepatic function.
Preclinical safety data
In conventional studies of repeated doses of moxifloxacin, hematological toxicity and hepatotoxicity were observed in animals. Central nervous system (CNS) toxicity was observed. These effects were observed after administration of high doses of moxifloxacin or after prolonged use.
High oral doses in animals (≥ 60 mg/kg), with plasma concentrations ≥ 20 mg/L, caused changes in electroretinogram parameters and, in some cases, retinal atrophy.
After intravenous administration, systemic toxicity was most pronounced when moxifloxacin was administered by bolus injection (45 mg/kg) and was not observed when moxifloxacin (40 mg/kg) was administered by slow infusion over 50 minutes. After intraarterial administration, inflammatory changes were observed with spread to periarterial soft tissues, indicating the need to avoid intraarterial administration of moxifloxacin.
In vitro, moxifloxacin at high concentrations affected the electrophysiological parameters of cardiac activity, which could cause prolongation of the QT interval. After intravenous administration of moxifloxacin to animals at a dose of 30 mg/kg by infusions lasting 15, 30 or 60 minutes, the degree of prolongation of the QT interval was observed to depend on the infusion rate: the shorter the infusion time, the more pronounced the prolongation of the QT interval. No prolongation of the QT interval was observed when a dose of 30 mg/kg was administered by infusion lasting 60 minutes.
When studying the effect of moxifloxacin on the reproductive function of animals, it was proven that moxifloxacin penetrates the placenta. Animal experiments did not reveal any teratogenic effect of moxifloxacin or impaired fertility after its use. In animals, a slight increase in the frequency of malformations of the spine and ribs was observed, but only in the case of a dose of 20 mg/kg intravenously, which was associated with a strong toxic effect on the mother's body. An increase in the number of cases of abortion in animals was observed against the background of therapeutic plasma concentrations predicted for use in humans.
Quinolones, including moxifloxacin, are known to cause damage to the cartilage of large diarthrodial joints in immature animals.
Indication
Community-acquired pneumonia
Complicated infectious diseases of the skin and subcutaneous tissues
Moxifloxacin should only be used when other antibacterial agents that are usually recommended for the initial treatment of these infections are inappropriate.
Official recommendations on the appropriate use of antibacterial agents should be taken into account.
Contraindication
– Hypersensitivity to moxifloxacin, other quinolone antibiotics or to any of the excipients of the drug;
– pregnancy or breastfeeding (see section “Use during pregnancy or breastfeeding”);
– childhood (up to 18 years old);
– history of tendon disease/pathology associated with the use of quinolones
During preclinical and clinical studies, changes in electrophysiological parameters of cardiac activity were observed after administration of moxifloxacin, manifested by prolongation of the QT interval. For this reason, moxifloxacin is contraindicated in patients with
– congenital or acquired prolongation of the QT interval;
– electrolyte imbalance, especially in the case of uncorrected hypokalemia;
– clinically significant bradycardia;
– clinically significant heart failure with reduced left ventricular ejection fraction;
– history of symptomatic arrhythmia
Moxifloxacin should not be used concomitantly with drugs that prolong the QT interval (see also section “Interaction with other medicinal products and other types of interactions”)
Due to insufficient clinical experience, moxifloxacin is contraindicated in patients with impaired liver function (Child-Pugh class C) and increased transaminase levels five times or more.
Special safety precautions
One vial of the medicinal product is intended for single use only. Unused solution should be discarded.
The following solutions have been found to be compatible with moxifloxacin 400 mg solution for infusion: water for injection; 0.9% sodium chloride solution; 1-molar sodium chloride solution; 5%, 10%, 40% glucose solution; 20% xylitol solution; Ringer's solution; complex sodium lactate solutions (Hartmann's solution, lactated Ringer's solution) Moxifloxacin solution for infusion should not be administered concomitantly with other medicinal products.
Do not use the medicine if there are visible solid impurities or if the solution is cloudy.
When stored in a cool place, a precipitate may form, which dissolves at room temperature. Therefore, it is not recommended to store the infusion solution at a temperature below 15 °C.
Interaction with other medicinal products and other types of interactions
Drug interactions
An additive effect of moxifloxacin and other medicinal products that can prolong the QTc interval cannot be excluded. This effect may lead to the development of ventricular arrhythmias, including polymorphic ventricular tachycardia of the pirouette type. For this reason, the use of moxifloxacin in combination with any of the following medicinal products is contraindicated (see also section "Contraindications")
– class IA antiarrhythmic drugs (e.g. quinidine, hydroquinidine, disopyramide);
– class III antiarrhythmic drugs (e.g. amiodarone, sotalol, dofetilide, ibutilide);
– antipsychotic drugs (e.g. phenothiazines, pimozide, sertindole, haloperidol, sultopride);
– tricyclic antidepressants;
– certain antimicrobials (saquinavir, sparfloxacin, erythromycin IV, pentamidine, antimalarials, including halofantrine);
– some antihistamines (terfenadine, astemizole, mizolastine);
Moxifloxacin should be administered with caution to patients taking medicinal products that may lower potassium levels (e.g. loop and thiazide diuretics, laxatives and enemas (in high doses), corticosteroids, amphotericin B), or medicinal products associated with clinically significant bradycardia.
After multiple doses of moxifloxacin in healthy volunteers, an increase in Cmax of digoxin by approximately 30% was observed without any effect on AUC or the level of the curve.
In studies involving volunteers with diabetes, simultaneous use of oral moxifloxacin and glibenclamide resulted in a decrease in Cmax of glibenclamide in blood plasma by approximately 21%. The combination of glibenclamide with moxifloxacin can theoretically provoke the development of minor short-term hyperglycemia. However, the observed changes in the pharmacokinetics of glibenclamide did not cause changes in pharmacodynamic parameters (blood glucose level, insulin level). Therefore, there is no clinically significant interaction between moxifloxacin and glibenclamide.
Change in the value of the international normalized ratio (INR)
There have been numerous reports of increased activity of oral anticoagulants in patients receiving antimicrobials, particularly fluoroquinolones, macrolides, tetracyclines, cotrimoxazole and some cephalosporins. Risk factors include infectious and inflammatory diseases, age and general condition of the patient. Therefore, it is difficult to determine whether the changes in INR are caused by infection or treatment. As a precautionary measure, INR can be checked more frequently. If necessary, appropriate adjustment of the oral anticoagulant dose should be made.
In clinical studies, the following substances have been shown to have no clinically significant interactions with moxifloxacin: ranitidine, probenecid, oral contraceptives, calcium supplements, parenteral morphine, theophylline, cyclosporine or itraconazole.
In vitro studies using human cytochrome P450 enzymes confirmed these results. Thus, metabolic interactions via cytochrome P450 enzymes are unlikely.
Interaction with food
Moxifloxacin does not show clinically significant interactions with food, including dairy products.
Application features
Moxifloxacin should be avoided in patients with a history of serious adverse reactions after the use of medicinal products containing quinolones or fluoroquinolones (see section "Adverse reactions"). Treatment of such patients with moxifloxacin should only be initiated in the absence of alternative therapy and after a careful assessment of the benefit/risk ratio (see also section "Contraindications").
The benefits of treatment with moxifloxacin, especially in the case of non-serious infections, should be assessed taking into account the information contained in this section.
QTc prolongation and clinical conditions in which QTc prolongation is possible Moxifloxacin has been shown to prolong the QTc interval on the electrocardiogram (ECG) in some patients. The extent of QT prolongation may increase with increasing plasma drug concentration during rapid intravenous infusion. Therefore, the recommendations for infusion duration should be followed, which should be at least 60 minutes, and the intravenous dose should not exceed 400 mg once daily. For more details, see sections “Contraindications” and “Interaction with other medicinal products and other types of interactions”
Moxifloxacin therapy should be discontinued if symptoms that may be associated with cardiac arrhythmia appear, regardless of whether this is confirmed by ECG results. Moxifloxacin should be used with caution in patients with conditions predisposing to the development of arrhythmia (e.g. acute myocardial ischemia), as such patients are at increased risk of ventricular arrhythmia (including polymorphic torsades de pointes) and cardiac arrest (see also sections “Contraindications” and “Interaction with other medicinal products and other types of interactions”). Moxifloxacin should be used with caution in patients taking medicinal products that may lower potassium levels (see also sections “Contraindications” and “Interaction with other medicinal products and other types of interactions”).
Moxifloxacin should be administered with caution to patients receiving medicinal products associated with clinically significant bradycardia (see also section "Contraindications"). Women and elderly patients may be more sensitive to the effects of medicinal products that prolong the QTc interval, such as moxifloxacin, and therefore such patients require special attention.
Hypersensitivity/allergic reactions
Cases of hypersensitivity and allergic reactions have been reported after the first use of fluoroquinolones, including moxifloxacin. Anaphylactic reactions can take the form of life-threatening shock even after the first use of the drug. In the event of clinical manifestations of severe hypersensitivity reactions, moxifloxacin should be discontinued and appropriate treatment should be initiated (e.g. shock therapy).
Cases of fulminant hepatitis, which may lead to hepatic failure, including fatal cases, have been reported with moxifloxacin (see section 4.8). In case of symptoms of fulminant hepatitis, such as rapidly progressive asthenia accompanied by jaundice, dark urine, bleeding tendency or hepatic encephalopathy, patients are advised to consult a doctor before continuing treatment. If signs of liver dysfunction appear, liver function tests should be performed.
Severe skin reactions
Severe cutaneous adverse reactions, including toxic epidermal necrolysis (TEN, also known as Lyell's syndrome), Stevens-Johnson syndrome (SJS) and acute generalised exanthematous pustulosis (AGEP), which can be life-threatening or fatal, have been reported with moxifloxacin (see section 4.8). Patients should be informed of the signs and symptoms of severe cutaneous reactions and monitored closely during treatment. If symptoms suggestive of these reactions occur, moxifloxacin should be discontinued immediately and alternative treatment considered. If a patient develops a serious reaction such as TENS, TEN or AGEP while taking moxifloxacin, moxifloxacin should never be restarted in this patient.
Patients prone to seizures
Quinolones are known to cause seizures. They should be administered with caution to patients with CNS disorders or other risk factors that may predispose to seizures or lower the seizure threshold. If seizures occur, moxifloxacin should be discontinued and appropriate measures taken.
Prolonged, disabling and potentially irreversible serious adverse reactions
Rare cases of prolonged (several months or years), disabling and potentially irreversible serious adverse reactions affecting various body systems (musculoskeletal, nervous system, mental and sensory) have been reported in patients treated with quinolones and fluoroquinolones, regardless of the patient's age and the presence of risk factors. Patients should be advised to immediately discontinue moxifloxacin at the first symptoms of any serious adverse reaction and seek medical advice.
Peripheral neuropathy
Cases of sensory or sensorimotor polyneuropathy resulting in paraesthesia, hypoesthesia, dysesthesia or weakness have been reported in patients treated with quinolones, including moxifloxacin. Patients taking moxifloxacin are advised to inform their doctor if they develop symptoms of neuropathy such as pain, burning, tingling, numbness or weakness before continuing treatment to prevent the development of irreversible conditions (see section 4.8).
Mental reactions
Psychiatric reactions may occur even after the first use of fluoroquinolones, including moxifloxacin. In rare cases, depression or psychiatric reactions have progressed to the development of suicidal thoughts and self-harm such as suicide attempts (see section "Adverse reactions"). If a patient develops such reactions, treatment with moxifloxacin should be discontinued and appropriate measures should be taken. Caution should be exercised when prescribing moxifloxacin to patients with a history of or current psychiatric disorders.
Antibiotic-associated diarrhea, including colitis
Cases of antibiotic-associated diarrhea (AAD) and antibiotic-associated colitis (AAC), including pseudomembranous colitis and Clostridium difficile-associated diarrhea, have been reported in association with the use of broad-spectrum antibiotics, including moxifloxacin. The severity of these events can range from mild diarrhea to fatal colitis. Therefore, it is important to consider the possibility of such a diagnosis in patients who develop severe diarrhea during or after the use of moxifloxacin. If AAD or AAC is suspected or confirmed, treatment with antimicrobials, including moxifloxacin, should be discontinued and appropriate therapeutic measures should be initiated immediately. In addition, appropriate infection control measures should be taken to reduce the risk of transmission. Medicinal products that inhibit peristalsis are contraindicated in patients who develop severe diarrhea.
Patients with myasthenia gravis
Moxifloxacin should be used with caution in patients with myasthenia gravis as its symptoms may be exacerbated.
During therapy with quinolones and fluoroquinolones, inflammation and tendon ruptures (especially of the Achilles tendon), sometimes bilateral, may occur, developing within 48 hours of starting treatment and may persist even for several months after stopping treatment (see sections “Contraindications” and “Adverse Reactions”). The risk of tendinitis and tendon rupture is increased in elderly patients, patients with renal insufficiency, patients with solid organ transplants and in patients receiving concomitant treatment with corticosteroids. Therefore, the concomitant use of the medicinal product with corticosteroids should be avoided.
At the first signs of tendinitis (e.g. painful swelling or inflammation), moxifloxacin should be discontinued and alternative therapy considered. Appropriate treatment of the affected limb should be initiated (e.g. immobilization). Corticosteroids should not be used if symptoms of tendinopathy develop.
Patients with renal impairment
Elderly patients with renal impairment should be given moxifloxacin with caution if they are unable to maintain adequate fluid intake, as dehydration increases the risk of renal failure.
Visual impairment
In case of visual impairment or any effect on the organs of vision, you should immediately seek advice from an ophthalmologist (see sections “Ability to influence the speed of reactions when driving vehicles or other mechanisms”, “Adverse reactions”)
Dysglycemia
As with all fluoroquinolones, cases of blood glucose abnormalities, both hypoglycemia and hyperglycemia, have been reported during treatment with moxifloxacin. Dysglycemia has occurred predominantly in elderly diabetic patients receiving oral hypoglycemic agents (e.g. sulfonylureas) or insulin concomitantly with moxifloxacin. Diabetic patients are advised to closely monitor their blood glucose levels (see section 4.8).
Prevention of photosensitivity reactions
Photosensitivity reactions have been reported in patients with quinolones. However, studies have shown that the risk of photosensitivity reactions with moxifloxacin is low. In any case, patients should avoid prolonged and/or intense exposure to sunlight or ultraviolet radiation during treatment with moxifloxacin.
Patients with glucose-6-phosphate dehydrogenase deficiency
Patients with glucose-6-phosphate dehydrogenase deficiency, as well as patients with a family history of this pathology, are prone to developing hemolytic reactions during treatment with quinolones. Therefore, moxifloxacin should be used with caution in this category of patients.
Inflammation of tissues in the periarterial area
Moxifloxacin solution for infusion is for intravenous use only. Intraarterial administration should be avoided as periarterial tissue inflammation has been observed in preclinical studies with this route of administration.
Patients with specific complicated skin and subcutaneous tissue infections
The clinical efficacy of moxifloxacin in the treatment of severe burn-related infections, fasciitis, and infected diabetic foot with osteomyelitis has not been established.
Aortic aneurysm and dissection and heart valve regurgitation/insufficiency
Epidemiological studies have shown an increased risk of aortic aneurysm and dissection, especially in the elderly, and of aortic and mitral valve regurgitation after the use of fluoroquinolones, especially in the elderly. Cases of aortic aneurysm and dissection, sometimes complicated by rupture (including fatal cases), and regurgitation/insufficiency of any of the heart valves have been reported in patients receiving fluoroquinolones.
Therefore, fluoroquinolones should only be used after careful benefit-risk assessment and after consideration of other treatment options in patients with a family history of aneurysm or congenital heart valve disease, in patients with a diagnosed aortic aneurysm or dissection, in patients with valvular heart disease, and in the presence of other risk factors such as
§ risk factors for the development of both aortic aneurysm and dissection, and heart valve regurgitation/insufficiency: connective tissue disorders such as Marfan syndrome or vascular Ehlers-Danlos syndrome, Turner syndrome, Behçet's disease, hypertension, rheumatoid arthritis;
§ risk factors for developing aortic aneurysm and dissection vascular disorders such as Takayasu arteritis or giant cell arteritis, atherosclerosis, Sjögren's syndrome;
§ risk factors for the development of regurgitation/heart valve insufficiency infective endocarditis
The risk of aortic aneurysm and dissection and rupture is increased in patients receiving concomitant systemic corticosteroids.
Patients should seek immediate emergency medical attention if they experience sudden abdominal, chest, or back pain.
Impact on biological tests
Moxifloxacin may interfere with the results of Mycobacterium spp tests by inhibiting mycobacterial growth, which may lead to false-negative results in patients taking moxifloxacin.
Infections caused by methicillin-resistant Staphylococcus aureus (MRSA)
Moxifloxacin is not recommended for the treatment of infections caused by methicillin-resistant Staphylococcus aureus. If MRSA infection is suspected or confirmed, treatment with an appropriate antibacterial agent should be initiated (see section 5.1).
Important information about excipients
This medicinal product contains 678.6 mg (approximately 29.52 mmol) of sodium per dose. Patients on a controlled salt diet should take this into account.
Use during pregnancy or breastfeeding
Pregnancy
The safety of moxifloxacin during pregnancy in humans has not been studied. The results of animal studies indicate reproductive toxicity (see section "Pharmacological properties") The potential risk for humans has not been established. Given the experimentally established risk of harmful effects of fluoroquinolones on weight-bearing cartilage in immature animals and taking into account the development of reversible joint lesions in children treated with some fluoroquinolones, moxifloxacin should not be prescribed to pregnant women (see section "Contraindications")
Breastfeeding period
There are no data on the use of the drug during breastfeeding. The results of preclinical studies indicate that small amounts of moxifloxacin penetrate into breast milk. Due to the lack of data on the effects on infants who are breastfed, and taking into account the experimental risk of harmful effects of fluoroquinolones on the cartilage of immature animals that bear the main load, breastfeeding is contraindicated during treatment with moxifloxacin (see section "Contraindications")
Fertility
Animal studies have not shown any effect on fertility (see section "Pharmacological properties")
Ability to influence reaction speed when driving vehicles or other mechanisms
Studies on the effect of moxifloxacin on the ability to drive and use machines have not been conducted. However, fluoroquinolones, including moxifloxacin, may affect the speed of reactions when driving or operating other mechanisms, causing CNS reactions (e.g. dizziness, acute temporary loss of vision) or acute short-term loss of consciousness (syncope) (see section "Adverse reactions"). Patients are advised to check their reaction to moxifloxacin before driving or operating other mechanisms.
Method of administration and doses
Dosage
Recommended dosage regimen 400 mg moxifloxacin as an infusion once daily Initial intravenous therapy may be continued with oral moxifloxacin tablets 400 mg if clinically indicated In clinical trials, most patients were switched to oral moxifloxacin within 4 days (communicable disease pneumonia) or 6 days (complicated skin and subcutaneous tissue infections) The recommended total duration of intravenous and oral treatment is 7–14 days for community-acquired pneumonia and 7–21 days for complicated skin and subcutaneous tissue infections
Method of administration and doses
The drug should be administered intravenously as a continuous infusion lasting at least 60 minutes (see also the section "Special instructions for use")
If indicated, the infusion solution can be administered via a T-catheter together with compatible infusion solutions (see section "Special precautions") Renal/hepatic impairment
Patients with mild to severe renal impairment and patients on chronic dialysis, such as those undergoing haemodialysis and long-term ambulatory peritoneal dialysis, do not require dose adjustment (for more details see section 5.1).
There is insufficient information in patients with hepatic impairment (see Contraindications).
Other special patient groups
Elderly patients and patients with
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.