Azithromycin 500 film-coated tablets 500 mg blister No. 3

Instructions Azithromycin 500 film-coated tablets 500 mg blister No. 3
Composition
active ingredient: azithromycin;
1 film-coated tablet contains azithromycin equivalent to 250 mg, 500 mg or 1000 mg of azithromycin anhydrous;
excipients:
Azithromycin 250: microcrystalline cellulose, calcium hydrogen phosphate, corn starch, povidone, magnesium stearate, talc, colloidal anhydrous silica, sodium lauryl sulfate, sodium starch glycolate (type A);
tablet shell: hydroxypropylmethylcellulose, titanium dioxide (E 171), iron oxide yellow (E 172);
Azithromycin 500: microcrystalline cellulose, corn starch, povidone, magnesium stearate, talc, colloidal anhydrous silica, sodium lauryl sulfate, sodium starch glycolate (type A);
tablet shell: hydroxypropylmethylcellulose, titanium dioxide (E 171), iron oxide yellow (E 172);
Azithromycin 1000: calcium hydrogen phosphate, corn starch, povidone, microcrystalline cellulose, magnesium stearate, talc, colloidal anhydrous silica, sodium starch glycolate (type A);
tablet shell: hydroxypropylmethylcellulose, polyethylene glycol 6000, titanium dioxide
(E 171), talc, iron oxide yellow (E 172).
Dosage form
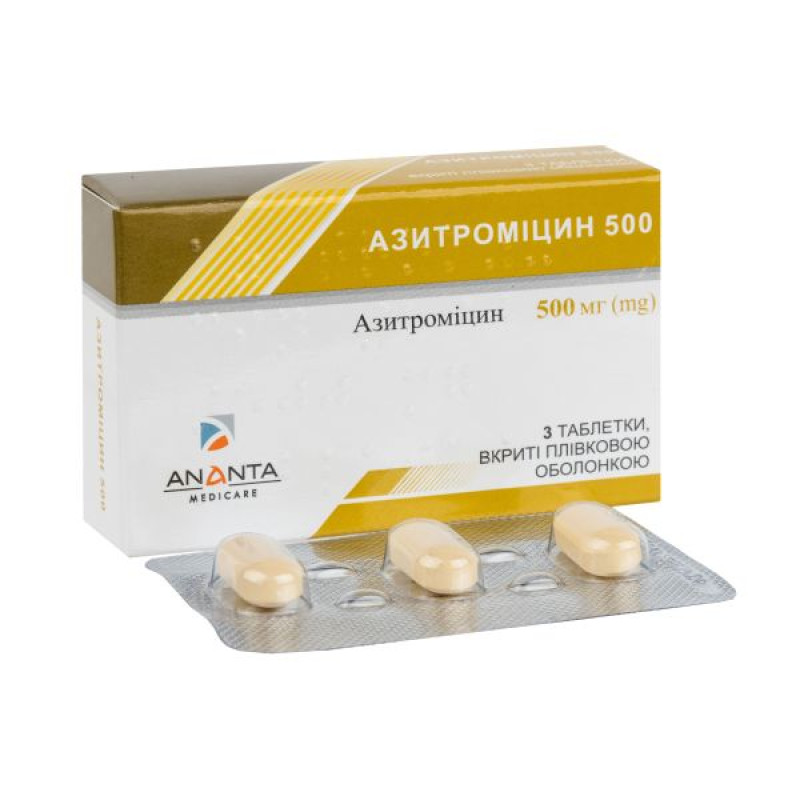
Film-coated tablets.
Main physicochemical properties:
250 mg tablets: yellow, round, biconvex, film-coated tablets;
500 mg tablets: yellow, oblong, biconvex, scored on one side and smooth on the other side, film-coated tablets;
1000 mg tablets: yellow, oblong, biconvex, scored on one side and smooth on the other side, film-coated tablets.
Pharmacotherapeutic group
Antibacterials for systemic use. Macrolides, lincosamides and streptogramins. Azithromycin. ATC code J01F A10.
Pharmacological properties
Pharmacodynamics.
Azithromycin is a macrolide antibiotic belonging to the azalide group. The molecule is formed by the introduction of a nitrogen atom into the lactone ring of erythromycin A. The mechanism of action of azithromycin is to inhibit bacterial protein synthesis by binding to
50S ribosomal subunit and inhibition of peptide translocation.
Mechanism of resistance
Complete cross-resistance exists among Streptococcus pneumoniae, group A beta-hemolytic streptococci, Enterococcus faecalis, and Staphylococcus aureus, including methicillin-resistant Staphylococcus aureus (MRSA), to erythromycin, azithromycin, other macrolides, and lincosamides.
The prevalence of acquired resistance may vary with location and time, therefore local information on resistance is necessary, especially when treating severe infections. Qualified advice may be sought if the local prevalence of resistance is such that the efficacy of the drug in the treatment of at least some types of infections is questionable.
| Typically sensitive species |
| Aerobic Gram-positive bacteria |
| Staphylococcus aureus (methicillin-susceptible) |
| Streptococcus pneumoniae (penicillin-sensitive) |
| Streptococcus pyogenes |
| Aerobic Gram-negative bacteria |
| Haemophilus influenzae |
| Haemophilus parainfluenzae |
| Legionella pneumophila |
| Moraxella catarrhalis |
| Pasteurella multocida |
| Anaerobic bacteria |
| Clostridium perfringens |
| Fusobacterium spp. |
| Prevotella spp. |
| Porphyromonas spp. |
| Other microorganisms |
| Chlamydia trachomatis |
| Chlamydia pneumoniae |
| Mycoplasma pneumoniae |
| Species that acquire resistance in isolated cases |
| Aerobic Gram-positive bacteria |
| Streptococcus pneumoniae with intermediate susceptibility to penicillin and penicillin-resistant |
| Inherently resistant microorganisms |
| Aerobic Gram-positive bacteria |
| Enterococcus faecalis |
| Staphylococci MRSA, MRSE* |
| Anaerobic bacteria |
| Bacteroides fragilis group |
The spectrum of antimicrobial action of azithromycin.
*Methicillin-resistant Staphylococcus aureus has a very high prevalence of acquired resistance to macrolides and has been listed here because of its rare susceptibility to azithromycin.
Pharmacokinetics.
Bioavailability after oral administration is approximately 37%. Maximum serum concentrations are reached 2–3 hours after administration.
When administered orally, azithromycin is distributed throughout the body. Pharmacokinetic studies have shown that the concentration of azithromycin in tissues is significantly higher (50 times) than in blood plasma, which indicates strong binding of the drug to tissues.
Serum protein binding varies with plasma concentrations and ranges from 12% at 0.5 μg/mL to 52% at 0.05 μg/mL in serum. The apparent volume of distribution at steady state (VVss) was 31.1 L/kg.
Approximately 12% of an intravenous dose of azithromycin is excreted unchanged in the urine over the next 3 days. Particularly high concentrations of unchanged azithromycin have been found in human bile. Also found in bile are 10 metabolites formed by N- and O-demethylation, hydroxylation of the desosamine and aglycone rings, and cleavage of the cladinose conjugate. Comparison of the results of liquid chromatography and microbiological analyses showed that the metabolites of azithromycin are not microbiologically active.
Indication
Infections caused by microorganisms sensitive to azithromycin:
- ENT infections (bacterial pharyngitis/tonsillitis, sinusitis, otitis media).
- Respiratory tract infections (bacterial bronchitis, community-acquired pneumonia).
- Skin and soft tissue infections: erythema migrans (initial stage of Lyme disease), erysipelas, impetigo, secondary pyodermatosis, acne vulgaris (common acne) of moderate severity.
- Sexually transmitted infections: uncomplicated genital infections caused by Chlamydia trachomatis.
Contraindication
Hypersensitivity to azithromycin, erythromycin, other macrolide and ketolide antibiotics, as well as to any other component of the drug.
Interaction with other medicinal products and other types of interactions
Antacids: When studying the effect of concomitant administration of antacids on the pharmacokinetics of azithromycin, there was generally no change in bioavailability, although the peak plasma concentration of azithromycin was reduced by approximately 25%. Azithromycin and antacids should not be taken simultaneously.
Cetirizine. In healthy volunteers, when administered concomitantly with azithromycin for
No pharmacokinetic interaction or significant changes in QT interval were observed after 5 days of cetirizine 20 mg at steady state.
Didanosine. When azithromycin 1200 mg daily is coadministered with didanosine
400 mg in six HIV-positive volunteers had no effect on the steady-state pharmacokinetics of didanosine compared to placebo.
Digoxin and Colchicine: Concomitant use of macrolide antibiotics, including azithromycin, with P-glycoprotein substrates such as digoxin and colchicine has been reported to result in increased serum levels of the P-glycoprotein substrate. Therefore, the possibility of increased serum substrate concentrations should be considered when azithromycin is coadministered with P-glycoprotein substrates such as digoxin.
Zidovudine. Single doses of 1000 mg and multiple doses of 1200 mg or 600 mg of azithromycin had little effect on the plasma pharmacokinetics or urinary excretion of zidovudine or its glucuronide metabolites. However, azithromycin increased the concentration of phosphorylated zidovudine, the clinically active metabolite, in peripheral blood mononuclear cells. The clinical significance of these findings is unknown but may be useful for patients.
Azithromycin does not have a significant interaction with the hepatic cytochrome P450 system. It is believed that the drug does not have the pharmacokinetic drug interactions characteristic of erythromycin and other macrolides. Azithromycin does not induce or inactivate hepatic cytochrome P450 through the cytochrome-metabolite complex.
Ergot: Due to the theoretical possibility of ergotism, the simultaneous administration of azithromycin with ergot derivatives is not recommended.
Pharmacokinetic studies have been conducted on the use of azithromycin and the following drugs, the metabolism of which occurs to a large extent with the participation of cytochrome P450.
Atorvastatin: Coadministration of atorvastatin (10 mg daily) and azithromycin (500 mg daily) did not alter plasma concentrations of atorvastatin (based on HMG CoA reductase inhibition assay). However, postmarketing cases of rhabdomyolysis have been reported in patients receiving azithromycin with statins.
Carbamazepine: In a pharmacokinetic interaction study in healthy volunteers, azithromycin had no significant effect on the plasma levels of carbamazepine or its active metabolites.
Cimetidine: In a pharmacokinetic study of the effect of a single dose of cimetidine (taken 2 hours before azithromycin) on the pharmacokinetics of azithromycin, no changes in the pharmacokinetics of azithromycin were observed.
Cyclosporine: A pharmacokinetic study in healthy volunteers given a 500 mg/day oral dose of azithromycin for 3 days followed by a single 10 mg/kg oral dose of cyclosporine demonstrated a significant increase in Cmax and AUC0-5 of cyclosporine. Therefore, caution should be exercised when these drugs are used concomitantly. If concomitant use of these drugs is necessary, cyclosporine levels should be monitored and the dose adjusted accordingly.
Efavirenz: Co-administration of a single dose of azithromycin 600 mg and efavirenz 400 mg daily for 7 days did not result in any clinically significant pharmacokinetic interaction.
Fluconazole: Coadministration of a single dose of 1200 mg azithromycin did not alter the pharmacokinetics of a single dose of 800 mg fluconazole. The total exposure and half-life of azithromycin were not altered by coadministration of fluconazole, but a clinically insignificant decrease in Cmax (18%) of azithromycin was observed.
Indinavir: Coadministration of a single dose of azithromycin 1200 mg had no statistically significant effect on the pharmacokinetics of indinavir administered at a dose of 800 mg.
3 times a day for 5 days.
Methylprednisolone: In a pharmacokinetic interaction study in healthy volunteers, azithromycin did not significantly affect the pharmacokinetics of methylprednisolone.
Midazolam: In healthy volunteers, co-administration of azithromycin 500 mg daily for 3 days did not cause clinically significant changes in the pharmacokinetics and pharmacodynamics of midazolam administered as a single 15 mg dose.
Nelfinavir. Concomitant administration of azithromycin (1200 mg) and nelfinavir at steady-state concentrations (750 mg 3 times a day) resulted in increased azithromycin concentrations. No clinically significant adverse events were observed, and no dose adjustment is necessary.
Rifabutin. Concomitant administration of azithromycin and rifabutin did not affect the serum concentrations of these drugs. Neutropenia has been observed in subjects receiving azithromycin and rifabutin concomitantly. Although neutropenia has been associated with rifabutin, a causal relationship to concomitant azithromycin has not been established.
Sildenafil: In healthy male volunteers, there was no evidence of an effect of azithromycin (500 mg daily for 3 days) on the AUC and Cmax of sildenafil or its major circulating metabolite.
Terfenadine: No pharmacokinetic interaction has been reported between azithromycin and terfenadine. In some cases, the possibility of such an interaction cannot be completely excluded, but there is no specific data on the existence of such an interaction.
Theophylline: There is no evidence of a clinically significant pharmacokinetic interaction when azithromycin and theophylline are coadministered in healthy volunteers.
Triazolam: Coadministration of azithromycin 500 mg on the first day and 250 mg on the second day with 0.125 mg of triazolam in healthy volunteers had no significant effect on all pharmacokinetic parameters of triazolam compared to triazolam and placebo.
Trimethoprim/sulfamethoxazole: Coadministration of double-strength trimethoprim/sulfamethoxazole (160 mg/800 mg) for 7 days with azithromycin 1200 mg on day 7 had no significant effect on the maximum concentration, total exposure, or urinary excretion of trimethoprim or sulfamethoxazole. Serum azithromycin concentrations were consistent with those observed in other studies.
Drugs that may prolong the QT interval: Azithromycin should be prescribed with caution to patients taking other drugs that may prolong the QT interval.
Application features
Hypersensitivity.
As with erythromycin and other macrolide antibiotics, rare serious allergic reactions, including angioedema and anaphylaxis (in isolated cases fatal), dermatological reactions, including acute generalized exanthematous pustulosis (AGEP), Stevens-Johnson syndrome, toxic epidermal necrolysis (TEN, rarely fatal), and drug reaction with eosinophilia and systemic symptoms (DRESS) have been reported (see section 4.8). Some of these reactions with azithromycin have resulted in recurrent symptoms and have required longer observation and treatment.
If an allergic reaction occurs, the drug should be discontinued and appropriate therapy should be initiated. The physician should be aware that allergic symptoms may recur after discontinuation of symptomatic treatment.
Liver dysfunction.
Since the liver is the primary route of elimination of azithromycin, caution should be exercised when prescribing azithromycin to patients with severe liver disease. Cases of fulminant hepatitis, resulting in life-threatening liver failure, have been reported with azithromycin. Some patients may have had a history of liver disease or were taking other hepatotoxic drugs.
If liver function impairment is detected, azithromycin should be discontinued.
Derivatives of ergot.
In patients taking ergot derivatives, the simultaneous use of some macrolide antibiotics contributes to the rapid development of ergotism. There is no data on the possibility of interaction between ergot and azithromycin. However, due to the theoretical possibility of ergotism, azithromycin should not be prescribed simultaneously with ergot derivatives.
Superinfections.
As with other antibiotics, observation for signs of superinfection due to non-susceptible organisms, including fungi, is recommended.
Clostridium difficile-associated diarrhea (CDAD) has been reported with nearly all antibacterial agents, including azithromycin, and has ranged in severity from mild diarrhea to fatal colitis. Antibacterial therapy alters the normal flora of the colon, leading to overgrowth of C. difficile.
Kidney dysfunction.
In patients with severe renal dysfunction (glomerular filtration rate <10 mL/min), a 33% increase in systemic exposure was observed when azithromycin was administered.
QT prolongation.
Prolonged cardiac repolarization and QT interval, which increased the risk of cardiac arrhythmia and ventricular fibrillation (torsade de pointes), have been observed with other macrolide antibiotics, including azithromycin. Since conditions associated with an increased risk of ventricular arrhythmias (including torsade de pointes) can lead to cardiac arrest, azithromycin should be administered with caution to patients with pre-existing proarrhythmic conditions (especially women and the elderly), including patients with:
- with congenital or registered prolongation of the QT interval;
- who are currently being treated with other active substances known to prolong the QT interval, such as antiarrhythmics of classes IA (quinidine and procainamide) and III (dofetilide, amiodarone and sotalol), cisapride and terfenadine, neuroleptics such as pimozide; antidepressants such as citalopram; and fluoroquinolones such as moxifloxacin and levofloxacin;
- with electrolyte imbalance, especially in the case of hypokalemia and hypomagnesemia;
- with clinically relevant bradycardia, cardiac arrhythmia or severe heart failure.
Myasthenia gravis.
Exacerbation of symptoms of myasthenia gravis or new development of myasthenic syndrome have been reported in patients receiving azithromycin therapy.
Streptococcal infections.
Azithromycin is generally effective in treating streptococcal infection of the oropharynx, but there are no data demonstrating the effectiveness of azithromycin in preventing acute rheumatoid arthritis.
Safety and efficacy for the prevention or treatment of Mycobacterium Avium Complex in children have not been established.
Use during pregnancy or breastfeeding
Pregnancy.
There are no adequate data on the use of azithromycin in pregnant women. In animal reproductive toxicity studies, azithromycin did not show teratogenic effects on the fetus, but the drug crossed the placenta. The safety of azithromycin during pregnancy has not been established. Therefore, azithromycin should be prescribed during pregnancy only if the benefit outweighs the risk.
Breast-feeding.
Azithromycin has been reported to pass into human milk, but adequate and well-controlled clinical studies to characterize the pharmacokinetics of azithromycin excretion into human milk have not been conducted. Azithromycin should be used during breastfeeding only if the expected benefit to the mother outweighs the potential risk to the child.
Fertility.
Fertility studies have been performed in rats; pregnancy rates were reduced following administration of azithromycin. The relevance of these findings to humans is unknown.
Ability to influence reaction speed when driving vehicles or other mechanisms
There is no evidence that azithromycin can impair the ability to drive or operate other mechanisms, but the possibility of developing adverse reactions such as delirium, hallucinations, dizziness, drowsiness, fainting, and seizures, which may affect the ability to drive or operate other mechanisms, should be taken into account.
Method of administration and doses
The drug should be used as a single daily dose, regardless of meals. If 1 dose of the drug is missed, the missed dose should be taken as soon as possible, and subsequent doses should be taken at intervals of 24 hours. Swallow the tablets without chewing.
Adults and children with a body weight ≥ 45 kg.
For infections of the ENT organs, respiratory tract, skin and soft tissues (except erythema migrans): the total dose is 1500 mg (500 mg 1 time per day). The duration of treatment is 3 days.
For erythema migrans: the total dose of azithromycin is 3 g, which should be taken according to the following scheme: 1 g on the first day, followed by 500 mg once a day from the 2nd to the 5th day.
For sexually transmitted infections: the recommended dose of azithromycin is
1 g once; course dose – 1 g.
Elderly patients.
Elderly patients do not need to change the dosage.
Since elderly patients may be at risk for cardiac conduction abnormalities, caution is recommended when using azithromycin due to the risk of cardiac arrhythmia and torsade de pointes.
Patients with renal impairment.
For patients with mild renal impairment (glomerular filtration rate
10–80 mL/min) the same dosage as for patients with normal renal function can be used. Azithromycin should be administered with caution to patients with severe renal impairment (glomerular filtration rate <10 mL/min).
Patients with liver dysfunction.
Since azithromycin is metabolized in the liver and excreted in the bile, the drug should not be used in patients with severe liver disease. Studies related to the treatment of such patients with azithromycin have not been conducted.
Children
The drug should be used in children weighing ≥ 45 kg. Children weighing ≤ 45 kg should be prescribed azithromycin in another dosage form, such as a suspension.
Overdose
Clinical experience with azithromycin suggests that adverse reactions occurring at higher than recommended doses are similar to those seen at usual therapeutic doses and may include diarrhea, nausea, vomiting, and reversible hearing loss.
In case of overdose, if necessary, administration of activated charcoal and general symptomatic and supportive treatment measures are recommended.
Adverse reactions
Frequency groups are defined using the following scale: very common (≥1/10); common (≥1/100 to <1/10); uncommon (≥1/1000 to <1/100); rare (≥1/10000 to <1/1000), very rare (<1/10000); not known (cannot be estimated from the available data). Within each frequency group, adverse reactions are presented in order of decreasing seriousness.
| System and organ class | Adverse reaction | Frequency |
| Infections and infestations | Candidiasis, vaginal infections, pneumonia, fungal infection, bacterial infection, pharyngitis, gastroenteritis, respiratory dysfunction, rhinitis, oral candidiasis | Infrequently |
| Pseudomembranous colitis | Unknown | |
| Blood and lymphatic system disorders | Leukopenia, neutropenia, eosinophilia | Infrequently |
| Thrombocytopenia, hemolytic anemia | Unknown | |
| On the part of the immune system | Angioedema, hypersensitivity reactions | Infrequently |
| Anaphylactic reaction | Unknown | |
| Metabolic | Anorexia | Infrequently |
| From the psyche | Nervousness, insomnia | Infrequently |
| Agitation | Rarely | |
| Aggression, anxiety, delirium, hallucinations | Unknown | |
| From the nervous system | Headache | Often |
| Dizziness, drowsiness, dysgeusia, paraesthesia | Infrequently | |
| Syncope, convulsions, hypoesthesia, psychomotor hyperactivity, anosmia, ageusia, parosmia, myasthenia gravis | Unknown | |
| From the organs of vision | Vision impairment | Infrequently |
| From the hearing organs | Hearing disorders, vertigo | Infrequently |
| Hearing impairment, including deafness and/or tinnitus | Unknown | |
| From the heart | Palpitation | Infrequently |
| Ventricular flutter/fibrillation (torsade de pointes), arrhythmia including ventricular tachycardia, ECG QT prolongation | Unknown | |
| From the vascular side | Tides | Infrequently |
| Arterial hypotension | Unknown | |
| From the respiratory system | Dyspnea, epistaxis | Infrequently |
| From the digestive tract | Diarrhea | Very often |
| Vomiting, abdominal pain, nausea | Often | |
| Constipation, flatulence, dyspepsia, gastritis, dysphagia, abdominal distension, dry mouth, eructation, mouth ulcers, salivary hypersecretion | Infrequently | |
| Pancreatitis, tongue discoloration | Unknown | |
| Hepatobiliary system | Liver dysfunction, cholestatic jaundice | Rarely |
| Hepatic failure (rarely fatal), fulminant hepatitis, hepatic necrosis | Unknown | |
| Skin and subcutaneous tissue disorders | Rash, pruritus, urticaria, dermatitis, dry skin, hyperhidrosis | Infrequently |
| Photosensitivity, acute generalized exanthematous pustulosis | Rarely | |
| Stevens–Johnson syndrome, toxic epidermal necrolysis, erythema multiforme, drug reaction with eosinophilia and systemic symptoms | ||
| Musculoskeletal system | Osteoarthritis, myalgia, back pain, neck pain | Infrequently |
| Arthralgia | Unknown | |
| From the urinary system | Dysuria, kidney pain | Infrequently |
| Acute renal failure, interstitial nephritis | Unknown | |
| Reproductive system and breast disorders | Uterine bleeding, testicular disorders | Infrequently |
| General disorders and local reactions | Oedema, asthenia, malaise, fatigue, facial oedema, chest pain, hyperthermia, pain, peripheral oedema | Infrequently |
| Laboratory indicators | Decreased lymphocyte count, increased eosinophil count, decreased blood bicarbonate, increased basophil count, increased monocyte count, increased neutrophil count | Often |
| Aspartate aminotransferase (AST) increased, alanine aminotransferase (ALT) increased, blood bilirubin increased, blood urea increased, blood creatinine increased, blood potassium changes, alkaline phosphatase increased, chloride increased, glucose increased, platelets increased, haematocrit decreased, bicarbonate increased, sodium abnormal | Infrequently | |
| Injury and poisoning | Complications after the procedure | Infrequently |
Information on adverse reactions possibly associated with the prevention and treatment of Mycobacterium Avium Complex is based on data from clinical trials and post-marketing surveillance. These adverse reactions differ in type or frequency from those reported with the immediate-release and long-release formulations.
Adverse reactions possibly related to prevention and treatment
| System and organ class | Adverse reaction | Frequency |
| Metabolic | Anorexia | Often |
| From the nervous system | Dizziness, headache, paresthesia, dysgeusia | Often |
| Hypoesthesia | Infrequently | |
| From the organs of vision | Vision impairment | Often |
| From the hearing organs | Deafness | Often |
| Hearing impairment, ringing in the ears | Infrequently | |
| From the heart | Palpitation | Infrequently |
| From the digestive tract | Diarrhea, abdominal pain, nausea, flatulence, gastrointestinal discomfort, frequent loose stools | Very often |
| Hepatobiliary system | Hepatitis | Infrequently |
| Skin and subcutaneous tissue disorders | Rash, itching | Often |
| Stevens–Johnson syndrome, photosensitivity | Infrequently | |
| Musculoskeletal system | Arthralgia | Often |
| General disorders and local reactions | Increased fatigue | Often |
| Asthenia, malaise | Infrequently |
Reporting of suspected adverse reactions.
Reporting suspected adverse reactions in the post-marketing period is an important measure. This allows for continued monitoring of the benefit/risk balance of the drug. Physicians are encouraged to report any suspected adverse reactions.
Expiration date
2 years.
Storage conditions
Store in the original packaging at a temperature not exceeding 30 ° C. Keep out of the reach of children.
Packaging
Azithromycin 250: 6 tablets in a blister, 1 blister in a cardboard box.
Azithromycin 500: 3 tablets in a blister, 1 blister in a cardboard box.
Azithromycin 1000: 4 tablets in a blister, 1 blister in a cardboard box.
Vacation category
According to the recipe.
Producer
Flamingo Pharmaceuticals Ltd.
Location of the manufacturer and address of its place of business
E-28, Opp. Fire Brigade, M.I.D.S., Taloja, Raigad District, Maharashtra, IN-410 208, India.
Applicant
Ananta Medicare Ltd.
Applicant's location
Suite 1, 2 Station Court, Imperial Wharf, Townmead Road, Fulham, London, United Kingdom.
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.