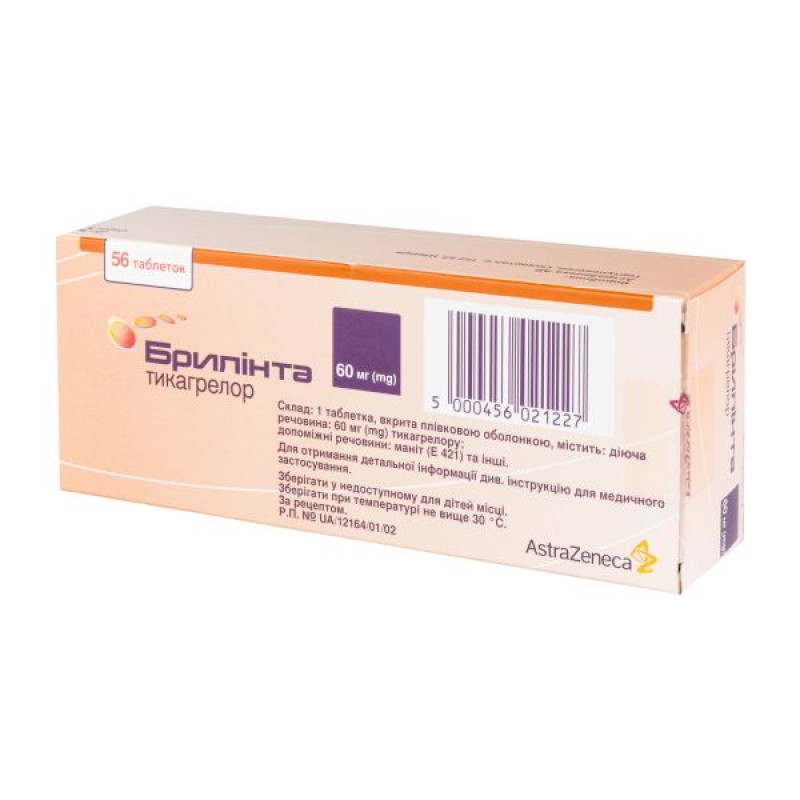
Brilinta film-coated tablets 60 mg blister No. 56

Instructions for Brilinta film-coated tablets 60 mg blister No. 56
Composition
active ingredient: ticagrelor;
1 film-coated tablet contains 60 mg of ticagrelor;
excipients: mannitol (E 421), calcium hydrogen phosphate, sodium starch glycolate, hydroxypropyl cellulose, magnesium stearate, hypromellose, titanium dioxide (E 171), polyethylene glycol 400, black iron oxide (E 172), red iron oxide (E 172).
Dosage form
Film-coated tablets.
Main physicochemical properties: pink, round, biconvex, film-coated tablets with engraving on one side and plain on the other.
Pharmacotherapeutic group
Antithrombotic agent. Platelet aggregation inhibitors, except heparin. ATC code B01A C24.
Pharmacological properties
Pharmacodynamics.
Mechanism of action
Brilinta contains ticagrelor, which belongs to the chemical class of cyclopentyltriazolopyrimidines (CTPs) and is an oral, selective, and reversible direct-acting P2Y12 receptor antagonist that prevents adenosine diphosphate (ADP)-mediated P2Y12-dependent platelet activation and aggregation. Ticagrelor does not prevent ADP binding, but by binding to the P2Y12 receptor, it prevents ADP-induced signaling. Since platelets are involved in the initiation and/or development of thrombotic complications of atherosclerosis, inhibition of platelet function has been shown to reduce the risk of cardiovascular events such as death, myocardial infarction (MI), or stroke.
Ticagrelor also increases local levels of endogenous adenosine by inhibiting the equilibrating nucleoside transporter subtype 1 (ENT-1).
Ticagrelor potentiates the following adenosine-induced effects in healthy subjects and in patients with acute coronary syndrome (ACS): vasodilation (as measured by increased coronary blood flow in healthy volunteers and patients with ACS; headache), inhibition of platelet function (in human whole blood in vitro), and dyspnea. However, the relationship between the observed increase in adenosine levels and clinical outcomes (e.g., morbidity-mortality) is not clearly established.
Pharmacodynamic effects
Start of action
In patients with stable coronary artery disease (CAD) receiving acetylsalicylic acid (ASA), the pharmacological effect of ticagrelor was rapid, as evidenced by a mean inhibition of platelet aggregation (PAA) of approximately 41% by ticagrelor 0.5 hours after a 180 mg loading dose, with a peak PAA effect of 89% at 2–4 hours post-dose, which was maintained for 2–8 hours. In 90% of patients, the final PAA at 2 hours post-dose was >70%.
End of action
If a coronary artery bypass graft (CABG) procedure is planned, the risk of bleeding in patients using ticagrelor is increased compared to those receiving clopidogrel if therapy is discontinued less than 96 hours before the procedure.
Data on switching from one drug to another
Switching from clopidogrel 75 mg to ticagrelor 90 mg twice daily resulted in an absolute increase in BP of 26.4%, and switching from ticagrelor to clopidogrel resulted in an absolute decrease in BP of 24.5%. Patients can be switched from clopidogrel to ticagrelor without interruption of the antiplatelet effect (see section “
Method of administration and doses
").
Clinical efficacy and safety
Clinical evidence of the efficacy and safety of ticagrelor was obtained in two phase 3 studies:
The PLATO [PLATelet Inhibition and Patient Outcomes] study compared ticagrelor and clopidogrel when used in combination with ASA and other standard therapy.
The PEGASUS TIMI-54 study [PrEvention with TicaGrelor of SecondAry Thrombotic Events in High-RiSk AcUte Coronary Syndrome Patients], which compared ticagrelor in combination with ASA and ASA treatment alone.
PLATO study (acute coronary syndrome)
The PLATO study included 18,624 patients who had symptoms of unstable angina, non-ST-segment elevation myocardial infarction, or ST-segment elevation myocardial infarction within the previous 24 hours and who were initially treated with medical therapy or PCI (percutaneous coronary intervention), CABG (coronary artery bypass grafting).
Clinical efficacy
In the setting of daily ASA, ticagrelor 90 mg twice daily was more effective than clopidogrel 75 mg daily in preventing the primary composite endpoint of cardiovascular death, myocardial infarction (MI), or stroke, due to the difference in rates of cardiovascular death and MI. Patients received a loading dose of 300 mg clopidogrel (possibly 600 mg in the case of PCI) or 180 mg ticagrelor.
The superior efficacy of ticagrelor compared with clopidogrel was consistently observed across multiple subgroups, regardless of body weight, gender, history of diabetes, transient ischemic attack or non-hemorrhagic stroke, or revascularization, concomitant medication including heparins, GpIIb/IIIa inhibitors, and proton pump inhibitors (see Interactions with other medicinal products and other forms of interaction). Efficacy was independent of the treatment modality chosen at randomization (invasive or medical), in both patients with unstable angina, non-ST-segment elevation myocardial infarction, and patients with ST-segment elevation myocardial infarction.
There was a weak regional drug interaction, with the hazard ratio (HR) for the primary endpoint favoring ticagrelor in the rest of the world but favoring clopidogrel in North America, which represented approximately 10% of the study population (p-value for interaction 0.045). Exploratory analysis suggests a possible dose-dependent interaction with ASA, as ASA efficacy was reduced with increasing ASA doses. ASA doses for continuous daily use with Brilinta should be 75–150 mg (see sections 4.2 and 4.4).
Treatment with Brilinta reduced the incidence of the primary composite endpoint compared with clopidogrel in both patients with unstable angina, non-ST-segment elevation MI, and patients with ST-segment elevation MI. Therefore, Brilinta 90 mg twice daily in combination with low-dose ASA can be prescribed to patients with ACS (unstable angina, non-ST-segment elevation myocardial infarction, or ST-segment elevation myocardial infarction), including patients undergoing medical therapy, percutaneous coronary intervention (PCI), or coronary artery bypass grafting (CABG).
PLATO genetic substudy
Genotyping of 10,285 patients for CYP2C19 and ABCB1 in the PLATO trial allowed us to establish the relationship between genotype groups and the results of the PLATO trial. The advantages of ticagrelor over clopidogrel in reducing the incidence of major cardiovascular events were not significantly dependent on the genotype of the patients. The overall incidence of major bleeding in the PLATO trial did not differ between the ticagrelor and clopidogrel groups, regardless of the genotype of the patients. The incidence of major bleeding not related to CABG, as defined by the PLATO trial, was increased with ticagrelor compared with clopidogrel in patients with one or more loss-of-function CYP2C19 alleles, but was similar to that with clopidogrel in patients without loss-of-function alleles.
A comprehensive component of efficiency and safety
The composite of efficacy and safety (cardiovascular death, myocardial infarction, stroke, or total major bleeding as defined by the PLATO study) indicates that the efficacy advantage of ticagrelor compared with clopidogrel is not offset by major bleeding events (ARV – 1.4%, VVD – 8%, HR 0.92; p = 0.0257) within 12 months after ACS.
Clinical safety
Holter additional study.
In the PLATO Holter monitoring study, more patients experienced episodes of ventricular asystole ≥ 3 seconds in the acute phase of acute coronary syndrome in the ticagrelor group than in the clopidogrel group; such episodes were more common in patients with chronic heart failure (CHF) compared with the general population; however, there was no statistically significant difference between the ticagrelor and clopidogrel groups at one month. No adverse clinical outcomes (including syncope or pacemaker implantation) due to this difference were observed in this patient population.
PEGASUS study (history of myocardial infarction)
The PEGASUS TIMI-54 study was a randomized, double-blind, placebo-controlled, parallel-group, international multicenter case-control study in 21,162 patients to evaluate the prevention of atherothrombotic events with ticagrelor at 2 doses (90 mg twice daily or 60 mg twice daily) in combination with low-dose ASA (75–150 mg) compared with ASA alone in patients with a history of MI and additional risk factors for atherothrombosis.
Patients were ineligible for the study if they were scheduled to receive a P2Y12 receptor antagonist, dipyridamole, cilostazol, or anticoagulant therapy during the study period; if they had a history of coagulation disorders or ischemic stroke or intracranial hemorrhage, a central nervous system tumor, or an intracranial vascular anomaly; if they had gastrointestinal bleeding within the previous 6 months, or if they had undergone major surgery within the previous 30 days.
Clinical efficacy
The ticagrelor 60 mg twice daily and 90 mg twice daily regimens in combination with ASA were more effective in preventing atherothrombotic events compared to ASA alone (composite endpoint: cardiovascular death, MI, and stroke) with a stable treatment effect throughout the study period, resulting in a relative risk reduction of 16% and an absolute risk reduction of 1.27% for ticagrelor 60 mg and 15% and 1.19%, respectively, for ticagrelor 90 mg.
Despite the similar efficacy profiles of the 90 mg and 60 mg doses, there is evidence that the lower dose is better tolerated and has a better safety profile with respect to the risk of bleeding and dyspnea. Therefore, only Brilinta 60 mg twice daily with concomitant ASA is recommended for the prevention of atherothrombotic events (cardiovascular death, MI, and stroke) in patients with a history of MI and at high risk of developing atherothrombotic events.
Relative to ASA alone, ticagrelor 60 mg twice daily significantly reduced the primary composite endpoint of cardiovascular death, MI, and stroke. The reduction in the primary composite endpoint was driven by a reduction in each component (17% CV death, 16% MI, and 25% stroke).
The composite endpoint OS was similar from day 1 to 360 (OS 17%) and from day 361 onwards (OS 16%). Data on the efficacy and safety of ticagrelor when treatment is continued beyond 3 years are limited.
There was no evidence of benefit (no reduction in the primary composite endpoint of cardiovascular death, MI and stroke, but an increase in major bleeding) of ticagrelor 60 mg twice daily in clinically stable patients more than 2 years after myocardial infarction or more than 1 year after discontinuation of previous ADP-receptor inhibitor treatment (see also section 4.2).
Clinical safety
The rate of premature discontinuation of ticagrelor 60 mg due to bleeding and dyspnea was higher in patients >75 years of age (42%) compared to younger patients (range: 23-31%), with a difference compared to placebo of more than 10% (42% vs. 29%) in patients >75 years of age.
Pharmacokinetics.
The pharmacokinetics of ticagrelor are linear, and exposure to ticagrelor and its active metabolite (AR-C124910XX) is approximately dose proportional up to 1260 mg.
Absorption
Ticagrelor is rapidly absorbed with a median tmax of approximately 1.5 hours. The formation of the major circulating metabolite of ticagrelor, AR-C124910XX (also active), occurs rapidly with a median tmax of approximately 2.5 hours. After a single oral dose of 90 mg ticagrelor in fasted healthy volunteers, Cmax was 529 ng/mL and AUC was 3451 ng*h/mL. The metabolite to parent ratio is 0.28 for Cmax and 0.42 for AUC. The pharmacokinetics of ticagrelor and AR-C124910XX in patients with a history of MI were generally similar to those observed in the ACS patient population. Based on the results of the population pharmacokinetic analysis of the PEGASUS study, the median Cmax of ticagrelor was 391 ng/mL and AUC was 3801 ng*h/mL at steady state when administered at a dose of 60 mg. For ticagrelor at a dose of 90 mg, the Cmax was 627 ng/mL and AUC was 6255 ng*h/mL at steady state.
The mean absolute bioavailability of ticagrelor was estimated to be 36%. Consuming a high-fat meal increased ticagrelor AUC by 21% and decreased Cmax of the active metabolite by 22%, but had no effect on Cmax of ticagrelor or AUC of the active metabolite. These small changes are considered to be of minimal clinical significance; therefore, ticagrelor can be administered without regard to food intake. Ticagrelor and its active metabolite are substrates of P-gp.
Ticagrelor crushed tablets mixed with water, when administered orally or via nasogastric tube into the stomach, have comparable bioavailability to whole tablets with respect to AUC and Cmax of ticagrelor and its active metabolite. Initial exposure (0.5 and 1 hour post-dose) of crushed and water-mixed ticagrelor tablets was higher than initial exposure of whole tablets, with generally similar concentration profiles over time (2–48 hours).
Distribution
The steady-state volume of distribution of ticagrelor is 87.5 L. Ticagrelor and its active metabolite are extensively bound to human plasma proteins (> 99.0%).
Biotransformation
The major metabolite of ticagrelor is AR-C124910XX, which is also active, as demonstrated by in vitro binding to platelet ADP-receptor P2Y12. The systemic exposure of the active metabolite is approximately 30–40% of the systemic exposure of ticagrelor.
Breeding
The primary route of elimination of ticagrelor is hepatic metabolism. When radiolabeled ticagrelor is administered, the mean level of radioactivity recovered is approximately 84% (57.8% in feces and 26.5% in urine). The urinary recovery of ticagrelor and the active metabolite was less than 1% of the dose. The primary route of elimination of the active metabolite is most likely biliary secretion. The mean t1/2 of ticagrelor was approximately 7 hours and that of the active metabolite was 8.5 hours.
Special patient groups
Elderly patients
Based on a population pharmacokinetic analysis, elderly patients (aged ≥ 75 years) with ACS had higher exposures to ticagrelor (approximately 25% for both Cmax and AUC) and the active metabolite than younger patients. These differences are not considered clinically relevant (see section 4.2).
Children
The use of ticagrelor in children has not been studied (see sections “Method of administration and dosage” and “Pharmacodynamics”).
Sex
Higher exposures of ticagrelor and the active metabolite were observed in women than in men. These differences are not considered clinically relevant.
Kidney dysfunction
Ticagrelor exposure was approximately 20% lower and the exposure of the active metabolite was approximately 17% higher in patients with severe renal impairment (creatinine clearance < 30 mL/min) than in patients with normal renal function (see section 4.2).
Liver dysfunction
Cmax and AUC of ticagrelor were 12% and 23% higher, respectively, in patients with mild hepatic impairment compared with healthy volunteers, but the effect of ticagrelor on AUC was similar in both groups. No dosage adjustment is required for patients with mild hepatic impairment. Ticagrelor has not been studied in patients with severe hepatic impairment; pharmacokinetic information is not available in patients with moderate hepatic impairment. In patients with moderate or severe elevations in one or more liver function tests at baseline, plasma concentrations of ticagrelor were on average similar to or slightly higher than in patients without baseline abnormalities.
Dosage adjustment is not required for patients with moderate hepatic impairment (see sections “Method of administration and dosage” and “Special warnings and precautions for use”).
Ethnicity
In Asian patients, the mean bioavailability was 39% higher than in Caucasian patients. In Black patients, the bioavailability of ticagrelor was 18% lower than in Caucasian patients; in a clinical pharmacology study, ticagrelor exposure (Cmax and AUC) in Japanese subjects was approximately 40% (20% after weight adjustment) higher than in Caucasian patients. Exposure in Hispanic or Latino patients was similar to that in Caucasian patients.
Indication
The use of Brilinta concomitantly with acetylsalicylic acid (ASA) is indicated for the prevention of atherothrombotic events in adult patients with
- acute coronary syndrome (ACS) or
- history of myocardial infarction (MI) and high risk of developing atherothrombotic events (see sections “Method of administration and dosage” and “Pharmacodynamics”).
Contraindication
Hypersensitivity to the active substance or to any of the excipients (see section "Adverse reactions").
Active pathological bleeding.
History of intracranial hemorrhage (see section "Adverse reactions").
Severe hepatic impairment (see sections “Method of administration and dosage”, “Special instructions for use” and “Pharmacokinetics”).
The concomitant use of ticagrelor with potent CYP3A4 inhibitors (e.g. ketoconazole, clarithromycin, nefazodone, ritonavir and atazanavir) is contraindicated as their co-administration may lead to a significant increase in ticagrelor exposure (see section 4.5).
Interaction with other medicinal products and other types of interactions
Ticagrelor is primarily a substrate of CYP3A4 and a moderate inhibitor of CYP3A4. Ticagrelor is also a substrate of P-glycoprotein (P-gp) and a weak inhibitor of P-gp and may increase the exposure of P-gp substrates.
Effects of other medicinal products on ticagrelor
Drugs metabolized by CYP3A4
Strong CYP3A4 inhibitors - Co-administration of ketoconazole and ticagrelor resulted in a 2.4-fold and 7.3-fold increase in ticagrelor Cmax and AUC, respectively. The Cmax and AUC of the active metabolite were decreased by 89% and 56%, respectively. Other strong CYP3A4 inhibitors (clarithromycin, nefazodone, ritonavir, and atazanavir) are expected to have similar effects, and therefore co-administration of strong CYP3A4 inhibitors with ticagrelor is contraindicated (see section 4.3). Moderate CYP3A4 inhibitors - Co-administration of diltiazem with ticagrelor resulted in a 69% increase in ticagrelor Cmax and 2.7-fold increase in AUC, and a 38% decrease in Cmax of the active metabolite, while its AUC remained unchanged. No effect of ticagrelor on diltiazem plasma levels was observed. Other moderate CYP3A4 inhibitors (e.g. amprenavir, aprepitant, erythromycin and fluconazole) are expected to have a similar effect and can therefore be used concomitantly with ticagrelor.
CYP3A4 inducers
Co-administration of rifampicin with ticagrelor resulted in a 73% and 86% decrease in ticagrelor Cmax and AUC, respectively. The Cmax of the active metabolite remained unchanged, while AUC was decreased by 46%. Other CYP3A inducers (e.g. phenytoin, carbamazepine and phenobarbital) are also expected to result in a decrease in ticagrelor exposure. Co-administration of ticagrelor with strong CYP3A inducers may result in a decrease in ticagrelor exposure and efficacy, and therefore their co-administration with ticagrelor is not recommended.
Cyclosporine (P-gp and CYP3A inhibitor)
Co-administration of cyclosporine (600 mg) and ticagrelor resulted in a 2.3- and 2.8-fold increase in ticagrelor Cmax and AUC, respectively. In the presence of cyclosporine, the AUC of the active metabolite increased by 32% and Cmax decreased by 15%.
There are no data on the concomitant use of ticagrelor with other active substances that are also strong P-gp inhibitors and moderate CYP3A4 inhibitors (e.g. verapamil, quinidine) and may lead to increased ticagrelor exposure. If the combination cannot be avoided, the concomitant use of these medicinal products should be undertaken with caution.
Others
Clinical pharmacology interaction studies have shown that co-administration of ticagrelor with heparin, enoxaparin, and ASA or desmopressin does not affect the pharmacokinetics of ticagrelor or its active metabolite, or ADP-induced platelet aggregation compared to ticagrelor alone. Medicinal products that affect hemostasis should be used with caution in combination with ticagrelor when clinically indicated.
A 2-fold increase in ticagrelor exposure was observed after daily consumption of large quantities of grapefruit juice (3 × 200 ml). This increase in exposure is not expected to be clinically relevant for most patients.
Effects of ticagrelor on other medicinal products
Drugs metabolized by CYP3A4
· Simvastatin - Co-administration of ticagrelor with simvastatin increased simvastatin Cmax by 81% and AUC by 56%, and increased simvastatin acid Cmax by 64% and AUC by 52% (in some cases, a 2- to 3-fold increase was observed). Co-administration of ticagrelor with simvastatin at doses above 40 mg/day may cause side effects of simvastatin, which should be weighed against the potential benefit. No effect of simvastatin on ticagrelor plasma levels was observed. Ticagrelor may have a similar effect on lovastatin. Co-administration of ticagrelor with simvastatin or lovastatin at doses above 40 mg is not recommended.
Atorvastatin - Co-administration of atorvastatin and ticagrelor increased the Cmax of atorvastatin acid by 23% and AUC by 36%. Similar increases in AUC and Cmax were observed for all metabolites of atorvastatin acid. This increase is not considered clinically significant.
· Similar effects on other statins metabolized by CYP3A4 cannot be excluded. Participants in the PLATO trial who received ticagrelor were taking a variety of statins, and 93% of these patients had no statin safety concerns.
Ticagrelor is a weak inhibitor of CYP3A4. Concomitant use of ticagrelor and CYP3A4 substrates with a narrow therapeutic index (e.g. cisapride or ergot alkaloids) is not recommended as ticagrelor may increase the exposure of these medicinal products.
P-gp substrates (including digoxin and cyclosporine)
Co-administration of ticagrelor increased digoxin Cmax by 75% and AUC by 28%. Mean trough digoxin levels increased by approximately 30% with co-administration of ticagrelor, and in some cases a maximum increase of 2-fold was observed. In the presence of digoxin, Cmax and AUC of ticagrelor and its active metabolite remained unchanged. Therefore, appropriate clinical and/or laboratory monitoring is recommended when P-gp-dependent drugs with a narrow therapeutic index, such as digoxin, are co-administered with ticagrelor.
No effect of ticagrelor on cyclosporine blood concentrations was observed. The effect of ticagrelor on other P-gp substrates has not been studied.
Drugs metabolized by CYP2C9
Co-administration of ticagrelor with tolbutamide did not alter the plasma levels of either drug, indicating that ticagrelor is not a CYP2C9 inhibitor and is therefore unlikely to affect the CYP2C9-mediated metabolism of drugs such as warfarin and tolbutamide.
Co-administration of ticagrelor with levonorgestrel and ethinyl estradiol increased ethinyl estradiol exposure by approximately 20% but did not alter the pharmacokinetics of levonorgestrel. No clinically significant effect on oral contraceptive efficacy is expected when levonorgestrel and ethinyl estradiol are co-administered with ticagrelor.
Drugs that can cause bradycardia
Since cases of mostly asymptomatic ventricular asystole and bradycardia have been observed, caution should be exercised when ticagrelor is used concomitantly with medicinal products that can induce bradycardia (see section 4.4). However, in the PLATO study, no clinically significant adverse reactions were observed after concomitant administration of one or more medicinal products that can induce bradycardia (e.g., 96% of patients were receiving concomitant beta-blockers, 33% were receiving calcium channel blockers diltiazem and verapamil, and 4% were receiving digoxin).
Other concomitant therapy
In clinical studies, ticagrelor was frequently used with ASA, proton pump inhibitors, statins, beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin receptor blockers for long periods of time as required by the patients' underlying conditions; and with heparin, low molecular weight heparin, and intravenous GpIIb/IIIa inhibitors for short periods of time (see section 5.1). No evidence of clinically significant adverse drug interactions with these medicinal products was observed.
Co-administration of ticagrelor with heparin, enoxaparin, or desmopressin did not affect activated partial thromboplastin time (aPTT), activated clotting time (ACT), or factor Xa assays. However, caution should be exercised when ticagrelor is administered concomitantly with medicinal products that may affect haemostasis due to potential pharmacodynamic interactions.
Due to reports of abnormal skin bleeding with selective serotonin reuptake inhibitors (SSRIs) (e.g. paroxetine, sertraline and citalopram), caution is recommended when SSRIs are used with ticagrelor as this may increase the risk of bleeding.
Application features
Risk of bleeding
The use of ticagrelor in patients with a known increased risk of bleeding should be weighed against the benefit of the drug in preventing atherothrombotic events (see sections 4.8 and 5.1). If clinically indicated, ticagrelor should be used with caution in the following patient groups:
Patients with a predisposition to bleeding (e.g. due to recent trauma or recent surgery, coagulation disorders, active or recent gastrointestinal bleeding). Ticagrelor is contraindicated in patients with active pathological bleeding, a history of intracranial hemorrhage, and patients with severe hepatic impairment (see section 4.3).
Patients who are concomitantly (within 24 hours of ticagrelor administration) taking medicinal products that may increase the risk of bleeding (e.g. nonsteroidal anti-inflammatory drugs (NSAIDs), oral anticoagulants and/or fibrinolytics).
Platelet transfusion did not reverse the antiplatelet effect of ticagrelor in healthy volunteers and is unlikely to be effective in treating patients with bleeding. Since concomitant use of ticagrelor with desmopressin did not result in a reduction in bleeding time by the template method, it is unlikely that desmopressin would be effective in treating clinical bleeding (see section 4.5).
The use of antifibrinolytic agents (aminocaproic acid or tranexamic acid) and/or recombinant factor VIIa may improve hemostasis. Ticagrelor may be resumed once the cause of bleeding has been identified and controlled.
Surgical intervention
Patients should be advised to inform their physicians and dentists that they are taking ticagrelor before planning any surgery and before taking any new medication.
In the PLATO study in patients undergoing coronary artery bypass grafting (CABG), ticagrelor had a higher incidence of bleeding than clopidogrel when therapy was discontinued 1 day before surgery, but major bleeding was observed at a similar rate to clopidogrel when therapy was discontinued 2 or more days before surgery (see section 4.8). If the patient requires elective surgery and the antiplatelet effect is undesirable, ticagrelor should be discontinued 7 days before surgery (see section 5.2).
Patients who have had an ischemic stroke
Patients with ACS who have had an ischemic stroke can be treated with Brilinta for up to 12 months (PLATO study).
The PEGASUS study did not include patients with a history of MI who had suffered an ischemic stroke. Therefore, due to the lack of data, treatment for more than one year in such patients is not recommended.
Ticagrelor is contraindicated in patients with severe hepatic impairment (see sections 4.2 and 4.3). There is limited experience with ticagrelor in patients with moderate hepatic impairment and caution is therefore recommended in such patients (see sections 4.2 and 4.2).
Patients at risk of bradycardia
Because of the previously reported cases of predominantly asymptomatic ventricular asystole, patients at increased risk of bradycardia (e.g., non-pacemaker patients with sick sinus syndrome, 2nd or 3rd degree atrioventricular block, or syncope due to bradycardia) were not included in the pivotal studies evaluating the safety and efficacy of ticagrelor. Therefore, due to limited clinical experience, ticagrelor should be used with caution in such patients (see section 5.1).
In addition, caution should be exercised when ticagrelor is co-administered with drugs that can cause bradycardia.
However, in the PLATO study, there was no evidence of clinically significant adverse reactions following concomitant use of one or more medicinal products known to induce bradycardia (e.g. 96% of patients were taking beta-blockers, 33% were taking the calcium channel blockers diltiazem and verapamil, and 4% were taking digoxin) (see section 4.5).
In the Holter substudy of the PLATO trial, episodes of ventricular asystole lasting ≥ 3 seconds during the acute phase of ACS were more frequently observed with ticagrelor than with clopidogrel. The increase in Holter-detected ventricular asystole episodes with ticagrelor was greater in patients with chronic heart failure (CHF) than in the general study population during the acute phase of ACS, but this difference was not observed after one month of treatment with ticagrelor or compared to clopidogrel. No adverse clinical outcomes associated with this difference (including syncope or the need for pacemaker implantation) were observed in this patient population (see section 5.2).
Dyspnea
Dyspnea has been reported in patients treated with ticagrelor. Dyspnea was usually mild to moderate and often resolved without the need for discontinuation of treatment. In patients with asthma/chronic obstructive pulmonary disease (COPD), the absolute risk of dyspnea with ticagrelor may be increased. Ticagrelor should be used with caution in patients with a history of asthma and/or COPD. The mechanism of this phenomenon is not known. If a patient reports the onset, duration, or worsening of dyspnea, a full evaluation should be performed and, if the patient is intolerant, ticagrelor should be discontinued. For detailed information, see section 4.8.
Increased creatinine levels
Creatinine levels may increase during treatment with ticagrelor. The mechanism of this phenomenon is not clear. Renal function should be monitored according to standard medical practice. In patients with ACS, it is also recommended to monitor renal function one month after starting ticagrelor treatment, with particular attention to patients ≥ 75 years of age, patients with moderate/severe renal impairment, and those concomitantly taking angiotensin receptor blockers (ARBs).
Increased uric acid levels
Hyperuricemia may occur during treatment with ticagrelor (see section 4.8). Caution should be exercised when treating patients with hyperuricemia or a history of gouty arthritis. Ticagrelor is not recommended for use in patients with uric acid nephropathy.
Other
Given the relationship between the maintenance dose of ASA and the relative efficacy of ticagrelor compared to clopidogrel observed in the PLATO study, the concomitant use of ticagrelor and high maintenance doses of ASA (> 300 mg) is not recommended (see section 5.1).
Premature termination
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.