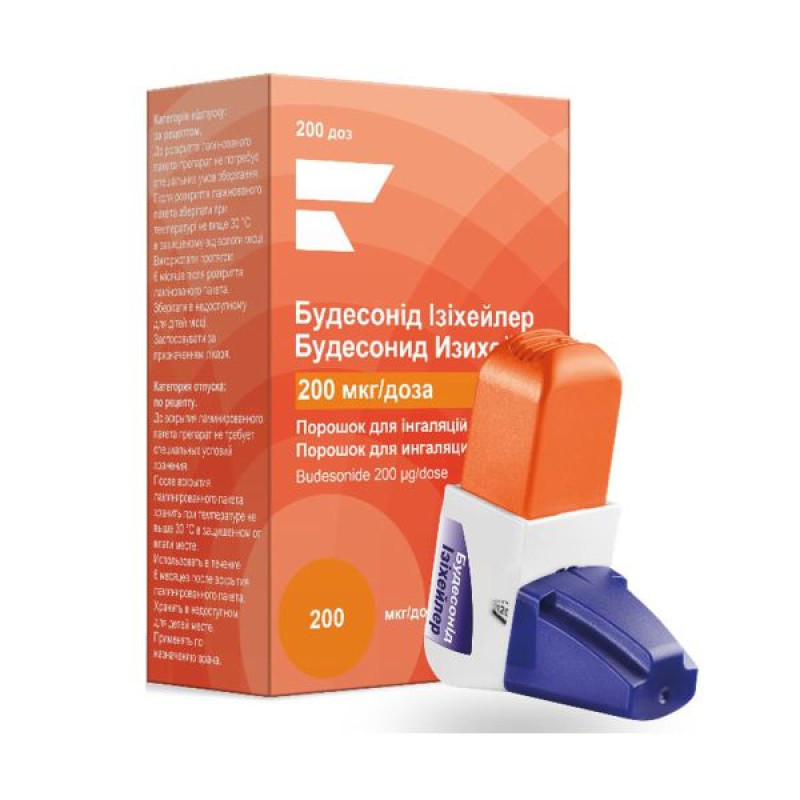
Budesonide Easyhaler inhalation powder 200 mcg/dose inhaler 200 doses
Pharmacological properties
Pharmacodynamics. Budesonide is a GCS with a powerful local anti-inflammatory effect.
Local anti-inflammatory effect. The exact mechanism of action of corticosteroids in the treatment of asthma has not been fully established. It is likely that anti-inflammatory effects, such as inhibition of the release of inflammatory mediators and inhibition of cytokine-mediated immune responses, may be important.
Onset of effect. After a single dose of budesonide administered by inhalation into the oropharynx using a dry powder inhaler, improvements in lung function are achieved within a few hours. After therapeutic use of budesonide administered by inhalation into the oropharynx using a dry powder inhaler, improvements in lung function have been shown to occur within 2 days of starting treatment, although it may take up to 4 weeks to achieve maximum effect.
Airway reactivity: Budesonide has also been shown to reduce airway reactivity to histamine and methacholine in hyperresponsive patients.
Exercise-induced asthma. Inhaled budesonide is effectively used for the prevention of exercise-induced asthma.
Function "hypothalamus - pituitary gland - adrenal cortex"
A study in healthy volunteers showed a dose-dependent effect of Budesonide Easyhaler on plasma and urinary cortisol levels. When used at recommended doses, budesonide has a lesser effect on adrenal cortex function than prednisone at a dose of 10 mg, as demonstrated by ACTH tests.
Children: Limited data from long-term studies suggest that most children and adolescents treated with inhaled budesonide eventually reach the expected adult height. However, there is an initial, small, temporary reduction in growth (approximately 1 cm). This generally occurs within the first year of treatment.
Slit-lamp examinations were performed in 157 children aged 5-16 years who received an average daily dose of 504 mcg for 3-6 years. The results were compared with those of 111 children with asthma of the same age group. Inhaled budesonide was not associated with an increased incidence of posterior subcapsular cataracts.
Pharmacokinetics. The activity of the drug Budesonide Easyhaler is determined by the original active substance - budesonide, which is a mixture of two epimers (22R and 22S). In studies of glucocorticoid receptor affinity, the 22R form has twice the activity as the 22S epimer. These two forms of budesonide are not subject to mutual transformation. The final T ½ for both epimers is the same (2-3 h). In patients with bronchial asthma, approximately 15-25% of the dose of budesonide used using the Easyhaler inhaler reaches the lungs. The largest part of the drug is retained in the oropharynx and swallowed if the mouth is not rinsed after inhalation.
Absorption. After oral administration of budesonide, peak plasma concentrations are reached after approximately 1-2 hours, and absolute systemic bioavailability is 6-13%. In plasma, 85-95% of budesonide is protein bound. After inhalation, C max in plasma is reached after 30 minutes. Most of the budesonide delivered to the lungs is absorbed into the systemic circulation.
Distribution: The volume of distribution is about 3 l/kg. Plasma protein binding is approximately 85-90%.
Metabolism and elimination. Budesonide is eliminated primarily by metabolism. Budesonide is rapidly and extensively metabolized in the liver by the cytochrome P450 3A4 system to form two major metabolites. The in vitro activity of these metabolites is less than 1% of that of the parent compound. Little metabolic inactivation has been observed in human lungs and blood.
Budesonide is excreted in the urine and feces in the form of conjugated and unconjugated metabolites.
Linearity. The pharmacokinetics of budesonide are dose proportional with respect to dosing.
Children. In children aged 4-6 years with bronchial asthma, the systemic clearance of budesonide is approximately 0.5 l/min. Per 1 kg of body weight in children, the clearance is approximately 50% higher than in adults. In children with asthma, the terminal T½ of budesonide after inhalation is approximately 2.3 hours. This is approximately the same as in healthy adults.
Certain patient groups: In patients with liver disease, the degree of bioavailability of budesonide may increase.
Indication
Persistent mild, moderate and severe asthma. Budesonide Easyhaler is not suitable for the treatment of acute asthma attacks.
Application
Method of administration: inhalation. To ensure an optimal response to treatment, budesonide easyhaler should be taken regularly. The therapeutic effect occurs a few days after starting the drug and reaches a maximum after several weeks of treatment.
When transferring patients to Budesonide Easyhaler from other inhalers, the treatment regimen should be selected individually. It is necessary to take into account the previous active substance, dosage and method of administration of the drug.
BA
The dosage of Budesonide Easyhaler should be selected individually.
The dose should always be reduced to the minimum necessary to ensure effective control of the course of asthma.
Adults (including the elderly) and adolescents aged 12 years and over: at the beginning of therapy, in severe asthma, when reducing the dose or when canceling oral GCS, the dose is 200-1600 mcg/day, divided into 2 inhalations.
Mild to moderate asthma: the dose is 200-800 mcg/day, divided into 2 inhalations. During periods of severe asthma, the daily dose may be increased to 1600 mcg, divided into 2 inhalations.
Children aged 5-12 years: the dose is 200-800 mcg/day, divided into 2 inhalations. During periods of severe asthma, the daily dose may be increased to 800 mcg.
Dosage 1 time per day
Adults (including the elderly) and adolescents aged 12 years and over: the dose is 200-800 mcg/day for mild to moderate asthma in patients who have not previously received inhaled corticosteroids.
For patients previously controlled with inhaled steroids (e.g. budesonide or beclomethasone dipropionate) administered twice daily, the dose may be increased to 800 mcg/day.
Children aged 5-12 years: the dose is 200-400 mcg/day for mild to moderate asthma in patients who have not previously received inhaled corticosteroids or whose disease is already controlled with inhaled steroids (e.g. budesonide or beclomethasone dipropionate) administered twice daily.
The patient should be transferred to inhalation of the drug 1 time per day at the same daily dose (taking into account the characteristics of the drug and the method of administration). After that, the dose should be reduced to the minimum necessary to ensure effective control of the course of asthma. Patients should be taught to take the drug 1 time per day, in the evening. It is important that the drug is taken regularly and at the same time in the evening.
There is insufficient data to develop recommendations for switching patients without prior inhaled GCS therapy to inhalation with Budesonide Easyhaler once daily.
Patients receiving the drug once a day should be advised to double the dose of their GCS by switching to inhalation twice a day if their asthma worsens (for example, if the frequency of bronchodilator use increases or if respiratory symptoms persist). In this case, patients should be advised to consult a doctor as soon as possible.
In the treatment of patients for whom an increased therapeutic effect is desired, an increased dose of Budesonide Easyhaler should usually be preferred to combination therapy with oral corticosteroids, since the risk of systemic side effects is lower with the use of Budesonide Easyhaler. The patient should always have a fast-acting inhaled bronchodilator available for the relief of asthma attacks.
Patients taking oral steroids. When switching from oral steroids to Budesonide Easyhaler, the patient should be in a relatively stable condition. A high dose of Budesonide Easyhaler should be used for 10 days in combination with the dose of oral steroid previously used. After this, the oral dose should be gradually reduced, for example by 2.5 mg prednisolone or equivalent per month to the lowest possible level. The oral steroid can often be stopped completely.
There is no experience in patients with impaired hepatic or renal function. Since budesonide is eliminated primarily by hepatic metabolism, an increased effect can be expected in patients with severe cirrhosis of the liver.
Operation and Care Instructions. The EasyHaler inhaler is flow-controlled. This means that when the patient inhales air through the mouthpiece, the medicinal substance enters the respiratory tract along with the air.
1. Remove the protective cap from the EasyHaler mouthpiece.
2. Shake the inhaler 3-5 times in an upright position.
3. To release the 1st dose of medication, place the Easyhaler between your thumb and forefinger and press the inhaler once. You will hear a click when you press.
4. Take a full breath, tightly cover the mouthpiece with your lips and inhale deeply, holding your breath for 5-10 seconds.
5. If more than 1 dose is prescribed, repeat steps 2, 3, and 4.
6. Close the EasyHaler mouthpiece with the protective cap.
It is important to draw the patient's attention to the following.
It is necessary to carefully read the operating instructions. After opening the laminated package, it is recommended to store the device in a protective container to protect it from shocks and ensure reliable operation of the device. Shake the device and activate it before each inhalation. In a sitting or standing position, inhale through the mouthpiece actively and deeply enough to ensure the optimal dose of the substance enters the bronchi. Do not exhale through the mouthpiece, as this will lead to a decrease in the delivered dose. If this still happens, you need to tap the inhaler on the table surface or on the palm of your hand to remove the powder from the mouthpiece, and then repeat the procedure for taking the drug. Do not activate the device more than 1 time without inhaling the powder. If this still happens, you need to tap the inhaler on the table surface or on the palm of your hand to remove the powder from the mouthpiece, and then repeat the procedure for taking the drug. Always put on the dust cap and close the protective container lid after using the inhaler to prevent accidental spraying of the powder from the device (which could lead to either an overdose or to inhaling an insufficient amount of the drug when the inhaler is used again). Rinse your mouth with water or brush your teeth after inhalation to minimize the risk of developing oropharyngeal candidiasis, as well as hoarseness. Clean the mouthpiece regularly with a dry tissue. You can use water for cleaning, as the powder is hygroscopic. Replace the Budesonide Easyhaler inhaler when the counter shows zero, even if some powder is still visible inside the device.Contraindication
Hypersensitivity to budesonide or lactose (which contains small amounts of milk proteins).
Side effects
Possible adverse reactions are presented by organ system and distributed according to the frequency of development: very common (≥1/10), common (≥1/100 to 1/10), uncommon (≥1/1000 to 1/100), rare (≥1/10,000 to 1/1000), very rare (1/10,000), frequency unknown (cannot be estimated from the available data).
Infectious and parasitic diseases: often - oropharyngeal candidiasis.
Immune system disorders: rarely - hypersensitivity reactions (including rash, contact dermatitis, urticaria, angioedema and anaphylactic reactions).
Endocrine disorders: rarely - hypocorticism, hypercorticism, signs and symptoms of systemic corticosteroid effects, including suppression of adrenal cortex function and growth retardation.
Mental disorders: rarely - depression, behavioral changes (mainly in children), anxiety, nervousness;
frequency unknown - psychomotor hyperactivity, sleep disorders, excitability, aggressiveness, irritability, psychosis.
Disorders of the organ of vision: very rarely - cataract, glaucoma.
Respiratory, thoracic and mediastinal disorders: often - cough, throat irritation; rarely - hoarseness, dysphonia, bronchospasm.
Digestive system disorders: often - difficulty swallowing.
Skin and subcutaneous tissue disorders: rarely - itching, erythema, hematoma.
Musculoskeletal and connective tissue disorders: very rare - decreased bone density.
Treatment with inhaled budesonide may lead to the development of candidal infection of the pharynx and oral cavity. Clinical experience shows that candidal infection develops less often if inhalation is carried out before meals and/or the mouth is rinsed after inhalation. In most cases, local antifungal drugs are effective in this disease, and treatment with inhaled budesonide does not need to be discontinued.
When taking inhaled corticosteroids, especially with prolonged use in high doses, systemic side effects may develop. Possible systemic side effects include: suppression of adrenal function, growth retardation in children and adolescents, decreased bone mineral density, cataracts, glaucoma, and susceptibility to infectious diseases. The ability to adapt to stress may be impaired. However, the likelihood of developing the described systemic side effects for the inhaled dosage form of budesonide is significantly lower than for orally administered corticosteroids.
Lactose - an excipient of the drug - contains a small amount of milk proteins, and therefore may cause allergic reactions.
Due to the risk of growth retardation in children and adolescents, the growth of patients should be monitored regularly.
Special instructions
Budesonide Easyhaler is not intended for the treatment of acute dyspnoea or status asthmaticus. These conditions require inhaled short-acting bronchodilators.
Adrenal dysfunction may occur in patients who have required acute high-dose corticosteroid therapy or who have been treated with inhaled corticosteroids at the highest recommended doses for a long period of time. These patients may develop signs and symptoms of adrenal insufficiency under stress. The need for additional systemic corticosteroid therapy should be considered during periods of stress and during elective surgery.
Adrenal dysfunction has been reported in patients with a history of oral corticosteroid dependence due to long-term systemic corticosteroid therapy. Recovery from oral corticosteroid therapy may take a long time, and therefore, when transferring patients with oral corticosteroid dependence to budesonide, there may be a risk of adrenocortical dysfunction for a long time. In such cases, regular monitoring of the hypothalamic-pituitary-adrenal axis function is necessary.
When switching from oral to inhaled budesonide, symptoms that were previously suppressed by systemic GCS therapy may develop, such as symptoms of allergic rhinitis, eczema, muscle and joint pain. To relieve such symptoms, in addition to therapy, specific treatment methods must be used.
Some patients may develop nonspecific malaise following withdrawal of systemic corticosteroids despite maintenance or even improvement of respiratory function. In such cases, patients should be strongly advised to continue inhaled budesonide and discontinue oral corticosteroids, despite clinical indications for withdrawal of inhaled corticosteroids, such as symptoms suggestive of adrenal insufficiency.
As with other inhalation therapy, paradoxical bronchospasm may occur, manifested by an immediate increase in wheezing and shortness of breath after inhalation of a dose of the drug. Paradoxical bronchospasm is relieved by rapid-acting inhaled bronchodilators and treatment should be initiated immediately. Budesonide should be discontinued immediately, the patient should be evaluated and, if necessary, alternative treatment should be instituted.
If an episode of acute dyspnoea occurs despite adequate treatment, a rapid-acting inhaled bronchodilator should be used and the prescribed treatment should be reviewed. In cases where asthma symptoms are not adequately controlled despite maximum doses of inhaled corticosteroids, patients may require a short course of systemic corticosteroids. In such situations, inhaled corticosteroid therapy should be supplemented with systemic agents.
Systemic effects of inhaled corticosteroids may occur, particularly when high doses are given for long periods, but are much less likely than those of oral corticosteroids. Possible systemic effects include Cushing's syndrome, Cushingoid features, adrenal suppression, growth retardation in children and adolescents, decreased bone mineral density, cataracts, glaucoma, and, much less commonly, various psychological and behavioral abnormalities, including psychomotor hyperactivity, sleep disturbances, anxiety, depression, or aggression (especially in children).
Therefore, it is important that the dose of inhaled corticosteroid is adjusted to the minimum level at which effective control of asthma is maintained.
In children receiving long-term therapy with inhaled corticosteroids, it is recommended to measure growth regularly. If growth is slowed, the treatment regimen should be reviewed with the aim of reducing the dose of inhaled corticosteroid to the lowest possible dose that provides effective control of asthma. In addition, the patient should be referred to a pediatric pulmonologist.
Oral candidiasis may occur during treatment with inhaled corticosteroids. To reduce the risk of oral candidiasis and hoarseness, patients should rinse their mouth thoroughly or brush their teeth after each use of inhaled corticosteroids. Oral candidiasis may require treatment with appropriate antifungal agents, and some patients may even need to discontinue inhaled corticosteroids.
Before starting therapy with Budesonide Easyhaler, patients with active or inactive pulmonary tuberculosis should be given appropriate specific treatment to ensure control of the disease. Similarly, patients with fungal, viral or other respiratory tract infections should be closely monitored and treated with specific therapy and Budesonide Easyhaler should only be used if adequate treatment for these infections is available.
Patients with excessive mucus secretion in the airways may require a short course of oral corticosteroid therapy.
Impaired liver function negatively affects the excretion of corticosteroids, reducing the rate of excretion and increasing systemic exposure, therefore, in such patients, the function of the hypothalamic-pituitary-adrenal cortex system should be regularly monitored.
Concomitant administration of ketoconazole, HIV protease inhibitors, and other potent CYP 3A4 inhibitors should be avoided. If this is not possible, the intervals between administration of the interacting drugs should be maximized.
Patients with rare hereditary syndromes of lactose intolerance, lactase deficiency (Lapp syndrome) or glucose-galactose malabsorption should not take this medicine.
Use during pregnancy and breastfeeding
Pregnancy. The results of a large prospective epidemiological study and worldwide post-marketing experience indicate that inhaled budesonide taken during pregnancy does not have a harmful effect on the health of the fetus/newborn. During pregnancy, the lowest effective dose of budesonide should be used, taking into account the risk of worsening asthma.
Breastfeeding. Budesonide is excreted in breast milk. Use in breastfeeding women should be considered only if the expected benefit to the woman outweighs any possible risk to the child.
Children: Do not use in children under 5 years of age.
The ability to influence the reaction speed when driving vehicles or other mechanisms. Does not affect.
Interactions
The metabolism of budesonide is primarily mediated by the CYP 3A4 isoenzyme. Therefore, inhibitors of this enzyme, such as itraconazole, ketoconazole, ritonavir, nelfinavir, cyclosporine, ethinylestradiol and troleandomycin, can increase the systemic effect of budesonide several times.
With short courses of therapy (1-2 weeks), this increase has little clinical significance, but with long-term use it should be taken into account.
Since there are no data on the necessary dosage in such cases, the combination of these drugs with budesonide should be avoided. If this is not possible, the interval between taking these drugs should be maximized and a reduction in the dose of budesonide should be considered.
Limited data indicate a significant increase in the level of budesonide in the blood plasma (on average 4-fold) with a single use of high doses of inhaled budesonide (1000 mcg) in combination with itraconazole 200 mg. Increased plasma concentrations of corticosteroids and increased their effect have been noted in women who were prescribed estrogens and steroid contraceptives simultaneously with corticosteroids, but no effect was recorded with budesonide therapy and concomitant use of combined oral contraceptives in low doses.
Due to the possibility of adrenal suppression, the ACTH stimulation test in the diagnosis of pituitary insufficiency may give false results (low values).
Overdose
Symptoms. The frequency of acute toxic reactions to budesonide is low. With prolonged use of the drug in excessively high doses, systemic reactions to GCS may occur, such as increased susceptibility to infections, the development of hypercorticism and adrenal suppression. Adrenal cortex atrophy and impaired ability to adapt to stress may occur.
Medical therapy in case of drug overdose. In case of acute overdose, even at excessive doses, clinical problems are not expected. Treatment with inhaled budesonide should be continued at the dose recommended for control of the course of asthma. The function of the "hypothalamus - pituitary - adrenal cortex" is restored after a few days.
In stressful situations, corticosteroids (e.g., high-dose hydrocortisone) may be necessary as a precautionary measure. Patients with adrenocortical atrophy are considered steroid-dependent and receive adequate maintenance therapy with systemic corticosteroids until the condition stabilizes.
Storage conditions
The drug does not require special storage conditions before opening the laminated package.
After opening the laminated package, store at a temperature not exceeding 30 °C in a place protected from moisture.
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.