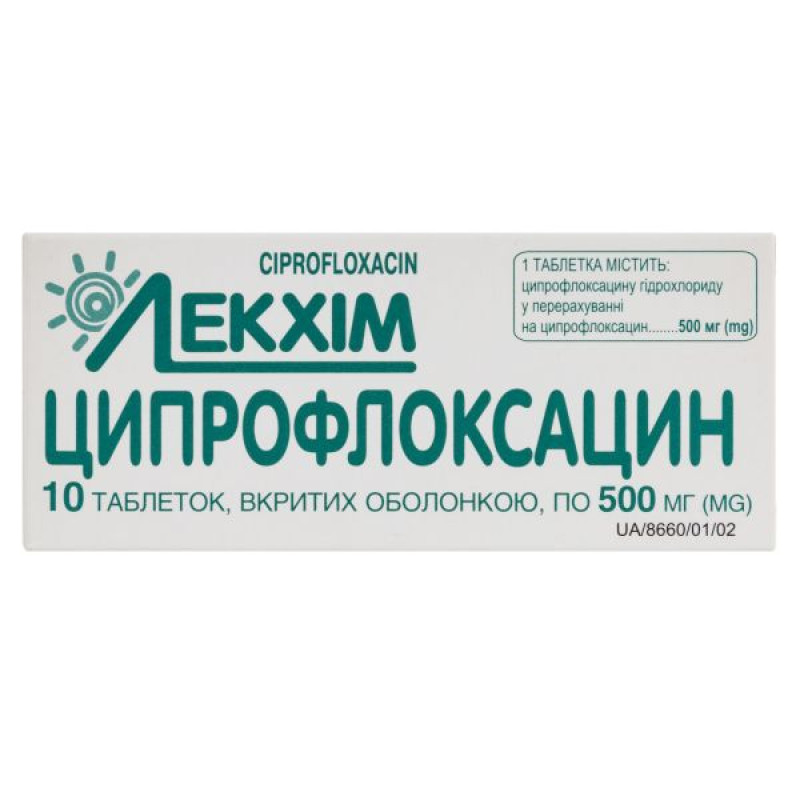
Ciprofloxacin film-coated tablets 500 mg blister No. 10

Instructions Ciprofloxacin film-coated tablets 500 mg blister No. 10
Composition
active ingredient: ciprofloxacin;
1 tablet contains ciprofloxacin hydrochloride equivalent to ciprofloxacin 250 mg;
1 tablet contains ciprofloxacin hydrochloride equivalent to ciprofloxacin 500 mg;
Excipients: microcrystalline cellulose, potato starch, corn starch, hypromellose (hydroxypropylmethylcellulose), talc, croscarmellose sodium, magnesium stearate, colloidal anhydrous silica, polyethylene glycol 6000 (macrogol 6000), titanium dioxide (E 171), polysorbate 80.
Dosage form
Film-coated tablets.
Main physicochemical properties: round, film-coated tablets, white or white with a yellowish tinge, with convex upper and lower surfaces. When broken, when viewed under a magnifying glass, a core surrounded by one continuous layer is visible.
Pharmacotherapeutic group
Antibacterials for systemic use. Fluoroquinolone group. ATX code J01M A02.
Pharmacological properties
Pharmacodynamics.
Ciprofloxacin is an antimicrobial drug of the fluoroquinolone group. The mechanism of action of ciprofloxacin is associated with the effect on DNA gyrase (topoisomerase) of bacteria, which plays an important role in the reproduction of bacterial DNA. Ciprofloxacin has a rapid bactericidal effect on microorganisms that are both dormant and multiplying.
The spectrum of action of the drug includes the following types of gram-negative and gram-positive microorganisms: E. coli, Shigella, Salmonella, Citrobacter, Klebsiella, Enterobacter, Serratia, Hafnia, Edwardsiella, Proteus (indole-positive and indole-negative), Providencia, Morganella, Providencia, Yersinia, Vibrio, Aeromonas, Plesiomonas, Pasteurella, Haemophilus, Campylobact, Pseudomonas, Legionella, Neisseria, Moraxella, Branhamella, Acinetobacter, Brucella, Staphylococcus, Streptococcus agalactiae, Listeria, Corynebacterium, Chlamydia, as well as plasmid forms of bacteria. Gardnerella, Flavobacterium, Alciligenes, Streptococcus pyogenes, Streptococcus pneumoniae, Streptococcus viridans, Mycoplasma hominis, Mycobacterium tuberculosis, Mycobacterium fortuitum show different sensitivity. Anaerobes, with some exceptions, are moderately sensitive (Peptococcus, Peptostreptococcus) or resistant (Bacteroides). Ciprofloxacin is effective against bacteria that produce β-lactamases. Ciprofloxacin is active against pathogens resistant to almost all antibiotics, sulfonamides and nitrofuran drugs. The most commonly resistant are: Streptococcus faecium, Ureaplasma uralyticum, Nocardia asteroides, Treponema pallidum. Resistance to the drug develops slowly and gradually.
Pharmacokinetics.
Ciprofloxacin is rapidly and well absorbed after oral administration (bioavailability is 50-85%). Maximum plasma concentrations are reached after 60-90 minutes. The volume of distribution is 2-3 l/kg. Binding to plasma proteins is insignificant (20-40%). Ciprofloxacin penetrates well into organs and tissues, bones. Approximately 2 hours after oral administration, it is found in tissues and body fluids in concentrations that are many times higher than its concentration in blood serum.
Ciprofloxacin is excreted from the body mainly unchanged: mainly by the kidneys (50-70%). The half-life from blood plasma after oral administration is from 3 to 5 hours. A significant amount of the drug is also excreted with bile and feces (up to 30%), so only significant renal dysfunction leads to a slowdown in excretion.
Indication
Ciprofloxacin is indicated for the treatment of the following infections (see sections 4.4 and 5.1). Before initiating therapy, special attention should be paid to all available information on resistance to ciprofloxacin.
Official recommendations on the appropriate use of antibacterial drugs should be taken into account.
Adults
Lower respiratory tract infections caused by gram-negative bacteria:
community-acquired pneumonia.
Exacerbation of chronic sinusitis, especially if caused by gram-negative bacteria*.
Middle ear infections (chronic suppurative otitis media).
Uncomplicated acute cystitis*.
Acute pyelonephritis.
Complicated urinary tract infections.
Bacterial prostatitis.
Gonococcal urethritis and cervicitis.
Epididymo-orchitis, particularly caused by Neisseria gonorrhoeae.
Pelvic inflammatory disease, particularly those caused by Neisseria gonorrhoeae.
In the above genital tract infections, when Neisseria gonorrhoeae is known or suspected as the causative agent, it is particularly important to obtain local information on ciprofloxacin resistance and confirm susceptibility based on laboratory tests.
Gastrointestinal tract infections (treatment of travelers' diarrhea).
Intra-abdominal infections.
Skin and soft tissue infections caused by gram-negative bacteria.
Bone and joint infections.
Fever in patients with neutropenia caused by bacterial infection.
Pulmonary form of anthrax (post-exposure prophylaxis and radical treatment).
*Only if other antibacterial agents commonly prescribed for the treatment of this infection are ineffective or inappropriate.
Children and adolescents
Complicated urinary tract infections and acute pyelonephritis. (In clinical studies, the age of children treated ranged from 1 to 17 years).
Pulmonary form of anthrax (post-exposure prophylaxis and radical treatment).
Treatment should only be initiated by a physician experienced in the treatment of cystic fibrosis and/or severe infections in children and adolescents (see sections 4.4 and 5.1).
Contraindication
Hypersensitivity to ciprofloxacin or other quinolone chemotherapeutic agents and other components of the drug; simultaneous use with tizanidine due to clinically significant side effects (arterial hypotension, drowsiness) associated with an increase in tizanidine concentration in blood plasma; glucose-6-phosphate dehydrogenase deficiency.
Interaction with other medicinal products and other types of interactions
Caution should be exercised when using ciprofloxacin simultaneously with class Ia or III antiarrhythmic drugs, tricyclic antidepressants, macrolides, antipsychotics, since ciprofloxacin has an additive effect on prolonging the QT interval (see section "Special warnings and precautions for use").
Chelation complex formation. When ciprofloxacin is administered orally with drugs containing multivalent cations, mineral supplements (e.g. calcium, magnesium, aluminium, iron), phosphate-binding polymers (e.g. sevelamer, lanthanum carbonate), sucralfate or antacids, as well as with drugs with a high buffer capacity (e.g. didanosine tablets) containing magnesium, aluminium or calcium, the absorption of ciprofloxacin is reduced. Therefore, ciprofloxacin should be taken either 1-2 hours before or 4 hours after taking these drugs.
This restriction does not apply to antacids belonging to the class of H2-receptor blockers.
Dairy and other foods. The concomitant use of ciprofloxacin and dairy or mineral-fortified foods (e.g. milk, yogurt, calcium-fortified orange juice) should be avoided. Other calcium-rich foods do not significantly affect the absorption of ciprofloxacin.
Probenecid. Probenecid slows down the biliary excretion of ciprofloxacin. Concomitant use of medicinal products containing probenecid and ciprofloxacin leads to an increase in the concentration of ciprofloxacin in the blood plasma. Probenecid affects the renal secretion of ciprofloxacin.
Metoclopramide: Metoclopramide accelerates the absorption of ciprofloxacin (when administered orally), resulting in a shorter time to reach maximum plasma concentrations. No effect on the bioavailability of ciprofloxacin was observed.
Omeprazole: Concomitant use of ciprofloxacin and omeprazole-containing medicinal products results in a slight decrease in Cmax and area under the concentration-time curve (AUC) of ciprofloxacin.
Tizanidine: Hypotensive and sedative adverse reactions are associated with increased serum concentrations of tizanidine. Therefore, concomitant use of ciprofloxacin and medicinal products containing tizanidine is contraindicated (see section 4.3).
Theophylline. Concomitant use of ciprofloxacin and medicinal products containing theophylline may lead to an undesirable increase in theophylline plasma concentrations, which may lead to the development of adverse reactions. In isolated cases, such adverse reactions may be life-threatening or fatal. If concomitant use of these drugs cannot be avoided, theophylline serum concentration should be monitored and the dose of theophylline reduced appropriately (see section 4.4).
Other xanthine derivatives: Increased serum concentrations of these xanthines have been reported following concomitant administration of ciprofloxacin and products containing caffeine or pentoxifylline (oxpentifylline).
Methotrexate. With simultaneous administration of ciprofloxacin, a slowdown in tubular transport (renal metabolism) of methotrexate is possible, which can lead to an increase in the concentration of methotrexate in the blood plasma. This may increase the likelihood of adverse toxic reactions caused by methotrexate. Simultaneous administration of ciprofloxacin and methotrexate is not recommended.
Nonsteroidal anti-inflammatory drugs. Animal studies have shown that the combined use of very high doses of quinolones (gyrase inhibitors) and some nonsteroidal anti-inflammatory drugs (except acetylsalicylic acid) can provoke seizures.
Vitamin K antagonists. Concomitant use of ciprofloxacin and a vitamin K antagonist may potentiate the anticoagulant effect of the latter. The degree of risk may vary depending on the underlying infection, age, and general condition of the patient, and it is difficult to accurately assess the effect of ciprofloxacin on the increase in the International Normalized Ratio (INR). Frequent monitoring of INR should be performed during and immediately after concomitant administration of ciprofloxacin and a vitamin K antagonist (warfarin, acenocoumarol, phenprocoumon, or fluindione). There have been reports of increased activity of oral anticoagulants in patients receiving antibacterial agents, including fluoroquinolones.
Duloxetine: Despite the lack of clinical data, the possibility of an interaction can be anticipated when ciprofloxacin and duloxetine are administered concomitantly (see section 4.4).
Ropinirole: Monitoring of ropinirole side effects and appropriate dose adjustment are recommended during and immediately after co-administration with ciprofloxacin (see section 4.4).
Lidocaine: Studies in healthy volunteers have shown that concomitant administration of lidocaine-containing medicinal products with ciprofloxacin, a moderate inhibitor of the CYP450 1A2 isoenzyme, results in a 22% decrease in the clearance of intravenously administered lidocaine. Although lidocaine is well tolerated, some interactions may occur following concomitant administration with ciprofloxacin, which may be associated with adverse reactions.
Clozapine: After concomitant administration of 250 mg ciprofloxacin with clozapine for 7 days, serum concentrations of clozapine and N-desmethylclozapine were increased by 29% and 31%, respectively. Clinical monitoring and appropriate dose adjustment of clozapine are recommended during and immediately after concomitant administration with ciprofloxacin (see section 4.4).
Sildenafil: In studies in healthy volunteers, Cmax and AUC of sildenafil were found to increase approximately two-fold after oral administration of 50 mg with 500 mg of ciprofloxacin. Ciprofloxacin should be administered concomitantly with sildenafil with caution, with a careful assessment of the risk-benefit ratio.
Phenytoin: Concomitant administration of ciprofloxacin and phenytoin may result in increased or decreased serum concentrations of phenytoin, therefore monitoring of drug levels is recommended.
Oral antidiabetic agents: Hypoglycaemia has been reported with concomitant administration of oral antidiabetic agents, particularly sulfonylureas (e.g. glibenclamide, glimepiride), which is probably due to ciprofloxacin potentiating the effects of oral antidiabetic agents (see section 4.8).
Application features
Ciprofloxacin should be avoided in patients who have had a serious adverse reaction to a quinolone or fluoroquinolone-containing drug in the past (see section 4.8). Ciprofloxacin should only be initiated in these patients if no alternative treatment options are available and after a careful benefit/risk assessment (see section 4.8).
The benefits of treatment with ciprofloxacin, especially in the case of non-serious infections, should be assessed taking into account the information contained in this section.
Prolonged, disabling and potentially irreversible serious adverse reactions.
Very rare cases of prolonged (months or years) disabling and potentially irreversible serious adverse reactions affecting various, sometimes multiple, body systems (musculoskeletal, nervous, mental and sensory) and existing risk factors have been reported in patients receiving quinolines and fluoroquinolones, regardless of age.
Ciprofloxacin should be discontinued immediately at the first signs or symptoms of any serious adverse reaction, and patients should be advised to seek medical advice.
Severe infections and/or infections caused by Gram-positive or anaerobic bacteria.
For the treatment of severe infections, infections caused by staphylococci or anaerobic bacteria, ciprofloxacin should be used in combination with appropriate antibacterial agents.
Pneumococci: Ciprofloxacin is not recommended for the treatment of pneumococcal infections due to insufficient efficacy against Streptococcus pneumoniae.
Urinary tract infections. Epididymo-orchitis and pelvic inflammatory disease may be caused by fluoroquinolone-resistant Neisseria gonorrhoeae. Ciprofloxacin should be administered concomitantly with other appropriate antibacterial agents, except in clinical situations that exclude ciprofloxacin-resistant strains of Neisseria gonorrhoeae. If clinical improvement does not occur after 3 days, therapy should be reviewed.
Cardiac disorders: Ciprofloxacin has been associated with prolongation of the QT interval on the electrocardiogram (see section 4.8). Elderly patients may be more sensitive to the effects of the drug on the QT interval. Ciprofloxacin should be used with caution in patients with concomitant medications that may prolong the QT interval (e.g., class Ia or III antiarrhythmics, tricyclic antidepressants, macrolides, antipsychotics) and in patients with risk factors for these conditions (e.g., history of QT prolongation, uncorrected hypokalemia).
Aortic aneurysm and dissection and regurgitation/valve insufficiency of the heart
Epidemiological studies have reported an increased risk of aortic aneurysm and dissection, especially in elderly patients, and of aortic and mitral valve regurgitation after the use of fluoroquinolones. Cases of aortic aneurysm and dissection, sometimes complicated by rupture (including fatal cases), and of regurgitation/insufficiency of any of the cardiac valves have been reported in patients receiving fluoroquinolones (see section 4.8).
Therefore, fluoroquinolones should only be used after careful benefit-risk assessment and after consideration of other therapeutic options in patients with a positive family history of aneurysm or congenital heart valve disease, or in patients with an existing diagnosis of aortic aneurysm and/or dissection, or heart valve disease, or in the presence of other risk factors or predisposing conditions.
both for aortic aneurysm and dissection, and for regurgitation/valve insufficiency (e.g. connective tissue disorders such as Marfan syndrome or Ehlers-Danlos syndrome, Turner syndrome, Behçet's disease, hypertension, rheumatoid arthritis) or additionally
in aortic aneurysm and dissection (e.g. vascular disorders such as Takayasu arteritis or giant cell arteritis, or known atherosclerosis, or Sjögren's syndrome) or additionally
in case of regurgitation/valvular insufficiency (e.g. infective endocarditis). The risk of aortic aneurysm and dissection and their rupture may be increased in patients receiving concomitant systemic corticosteroids.
Patients should seek immediate medical attention in the emergency department if they experience sudden abdominal, chest, or back pain.
Patients should be advised to seek immediate medical attention in the event of acute shortness of breath, new onset of palpitations, or development of abdominal or lower extremity edema.
Children and adolescents. Analysis of the available safety data on the use of ciprofloxacin in children, most of whom had cystic fibrosis, did not provide any evidence of treatment-related cartilage or joint damage. The use of ciprofloxacin for indications other than the treatment of pulmonary complications caused by Pseudomonas aeruginosa in children with cystic fibrosis (aged 5-17 years), the treatment of complicated urinary tract infections and pyelonephritis caused by E. coli (aged 1-17 years), and post-exposure anthrax have not been studied. Clinical experience with ciprofloxacin in children for other indications is limited.
The use of ciprofloxacin in children and adolescents should be in accordance with current official guidelines. Treatment with ciprofloxacin should only be initiated by a physician experienced in the management of children and adolescents with cystic fibrosis and/or severe infections.
Hypersensitivity to the drug. In some cases, hypersensitivity and allergic reactions may occur after the first use of ciprofloxacin, which should be reported to the doctor immediately.
In rare cases, anaphylactic/anaphylactoid reactions may progress to a state of shock that is life-threatening. In some cases, they have been observed after the first use of ciprofloxacin. In these cases, ciprofloxacin should be discontinued and medical treatment (treatment of anaphylactic shock) should be initiated immediately.
Gastrointestinal tract. In case of severe and persistent diarrhea during or after treatment, the doctor should be informed, as this symptom may mask a serious gastrointestinal disease (e.g. pseudomembranous colitis, which can be life-threatening and possibly fatal), which requires immediate treatment. In such cases, ciprofloxacin should be discontinued and appropriate therapy should be initiated (e.g. vancomycin orally 4×250 mg/day). Medicinal products that inhibit peristalsis are contraindicated.
Clostridium difficile produces toxins A and B, which contribute to the development of antibiotic-associated diarrhea. Clostridium difficile produces large amounts of the toxin, causing increased morbidity and mortality due to possible resistance to antimicrobial therapy and the need for colectomy. The possibility of antibiotic-associated diarrhea due to Clostridium difficile should be considered in all patients with diarrhea after antibiotic use. A careful medication history is necessary, as antibiotic-associated diarrhea due to Clostridium difficile may develop within two months of antibiotic administration. If a diagnosis of antibiotic-associated diarrhea due to Clostridium difficile is considered or confirmed, the use of antibiotics that are not active against Clostridium difficile may need to be discontinued. Depending on clinical data, it is necessary to correct the water and electrolyte balance, consider the need for additional protein supplements, use antibacterial drugs to which Clostridium Difficile is sensitive. Surgical intervention may also be necessary.
Cases of hepatic necrosis and life-threatening hepatic failure have been reported with ciprofloxacin. If any signs and symptoms of liver disease (such as anorexia, jaundice, dark urine, pruritus, or abdominal tenderness) occur, treatment should be discontinued. Transient increases in transaminases, alkaline phosphatase, and cholestatic jaundice may also occur, especially in patients with pre-existing liver disease.
Musculoskeletal system. In general, ciprofloxacin should not be used in patients with tendon diseases and disorders associated with the use of quinolines in history. However, in rare cases, after microbiological examination of the pathogen and an assessment of the benefit/risk ratio, ciprofloxacin may be prescribed to these patients for the treatment of certain severe infections, namely in cases of failure of standard therapy or bacterial resistance, when the results of microbiological examinations justify the use of ciprofloxacin. Tendinitis or tendon rupture (especially of the Achilles tendon), sometimes bilateral, may occur with ciprofloxacin during the first 48 hours of treatment. The risk of tendinopathy may be increased in elderly patients or in patients receiving concomitant corticosteroids (see section "Adverse reactions"). If any signs of tendinitis (e.g. painful swelling, inflammation) occur, ciprofloxacin should be discontinued. The affected limb should be kept at rest.
Nervous system: Patients with epilepsy and patients with a history of central nervous system dysfunction (e.g., lowered seizure threshold, history of seizures, decreased cerebral blood flow, changes in brain structure, or stroke) should only take ciprofloxacin if the expected benefit outweighs the potential risk, as these patients are at risk for possible central nervous system adverse reactions.
In some cases, adverse reactions from the central nervous system are observed after the first use of ciprofloxacin. In rare cases, depression or psychosis may progress to a life-threatening condition. In such cases, ciprofloxacin should be discontinued and a doctor should be immediately informed.
Peripheral neuropathy
Cases of sensory or sensorimotor polyneuropathy resulting in paresthesia, hypoesthesia, dysesthesia or weakness have been reported in patients receiving quinolones, including ciprofloxacin. Patients receiving ciprofloxacin are advised to inform their physician of the development of symptoms of neuropathy such as pain, burning, tingling, numbness or weakness before continuing treatment to prevent the development of irreversible conditions (see section "Adverse Reactions").
Skin and subcutaneous tissue: Ciprofloxacin has been shown to cause photosensitivity reactions, therefore patients taking ciprofloxacin should avoid intense sunlight or ultraviolet radiation. If photosensitivity reactions (similar to sunburn) occur, ciprofloxacin therapy should be discontinued.
Cytochrome P450. Ciprofloxacin is known to be a moderate inhibitor of cytochrome P450 1A2 enzymes. Caution should be exercised when ciprofloxacin is co-administered with drugs that are metabolized by a similar enzyme pathway (such as theophylline, methylxanthines, caffeine, duloxetine, clozapine). Increased serum concentrations of these drugs are associated with inhibition of their metabolic clearance by ciprofloxacin, which may lead to specific side effects.
As with all quinolones, changes in blood glucose levels, including cases of hypoglycaemia, have been reported, as well as cases of hyperglycaemia, usually in diabetic patients receiving concomitant oral hypoglycaemic therapy (e.g. glibenclamide) or insulin. Cases of hypoglycaemic coma have been reported. Close monitoring of blood glucose levels is recommended in diabetic patients (see section 4.8).
Effect on laboratory test results: Ciprofloxacin may interfere with the results of Mycobacterium spp. cultures in vitro by inhibiting the growth of mycobacterial cultures, which may lead to false-negative results in cultures from patients taking ciprofloxacin.
Ciprofloxacin should not be used as monotherapy for the treatment of severe infections caused by Gram-positive or anaerobic bacteria.
Traveler's diarrhea.
When choosing ciprofloxacin, information on ciprofloxacin resistance of relevant microorganisms in the countries visited by the patient should be taken into account.
Bone and joint infections.
Ciprofloxacin should be used in combination with other antimicrobial agents depending on the results of microbiological testing.
Pulmonary form of anthrax.
Use in humans is based on in vitro susceptibility data, animal studies, together with limited human data. The physician should follow national and/or international protocols for the treatment of anthrax.
Ciprofloxacin should be used with caution in patients with myasthenia gravis.
The simultaneous administration of ciprofloxacin and methotrexate is not recommended.
Bronchopulmonary infections in cystic fibrosis. Clinical trials have included children and adolescents aged 5-17 years. There is more limited experience in the treatment of children aged 1 to 5 years.
Complicated urinary tract infections and pyelonephritis. Treatment of urinary tract infections with ciprofloxacin should be considered when other treatment options are not available. Treatment should be based on microbiological findings.
Tendinitis and tendon rupture.
Tendinitis and tendon rupture (not limited to the Achilles tendon), sometimes bilateral, may occur as early as 48 hours after initiation of treatment with quinolones and fluoroquinolones and even up to several months after discontinuation of treatment. The risk of tendinitis and tendon rupture is increased in elderly patients, patients with renal impairment, patients with solid organ transplantation and patients receiving concomitant corticosteroids. Therefore, concomitant use of corticosteroids should be avoided.
At the first signs of tendinitis (e.g. painful swelling, inflammation), treatment with the drug should be discontinued and alternative treatment should be considered. The affected limb(s) should be treated appropriately (e.g. immobilization). Corticosteroids should not be used if signs of tendinopathy occur.
Kidneys and urinary system: Crystalluria has been reported in association with the use of ciprofloxacin. Patients taking ciprofloxacin should be adequately hydrated. Excessive alkalinity of the urine should be avoided.
Resistance: During or after a course of treatment with ciprofloxacin, resistant bacteria may be isolated with or without clinically apparent superinfection. There may be a certain risk of isolation of ciprofloxacin-resistant bacteria during long courses of treatment and in the treatment of nosocomial infections and/or infections caused by Staphylococcus and Pseudomonas species.
Use during pregnancy or breastfeeding
Ciprofloxacin should not be used in pregnant and breastfeeding women, given the lack of experience with its use in this category of patients.
Given the data from animal studies, the possibility of damage to articular cartilage in newborns cannot be completely ruled out, while the possibility of teratogenic effects (malformations) has not been confirmed.
Breastfeeding period.
Ciprofloxacin passes into breast milk. Due to the potential risk of damage to articular cartilage in newborns, ciprofloxacin should not be used during breastfeeding.
Ability to influence reaction speed when driving vehicles or other mechanisms
Even when taken exactly as directed by your doctor, this medicine may affect your reaction time, which may interfere with your ability to drive or operate machinery. This is especially true when taken with alcohol.
Method of administration and doses
The dose should be determined according to the indication, severity and site of the infection, the sensitivity of the causative organism(s) to ciprofloxacin, the patient's renal function, and in children and adolescents - according to body weight.
The duration of treatment depends on the severity of the disease, the characteristics of the clinical picture, and the type of pathogen.
Treatment of some infections (e.g. pelvic inflammatory disease, intra-abdominal infections, infections in neutropenic patients, bone and joint infections) may require concomitant administration of other necessary antibacterial agents depending on the type of pathogens identified.
Adults
| Indication | Daily dose, mg | Total duration of treatment (may include initial parenteral administration of ciprofloxacin) | |
|---|---|---|---|
| Lower respiratory tract infections caused by gram-negative bacteria | Community-acquired pneumonia | 500 mg twice daily to 750 mg twice daily | 7 -14 days |
| Upper respiratory tract infections | Exacerbation of chronic sinusitis, especially if caused by gram-negative bacteria | 500 mg twice daily to 750 mg twice daily | 7 -14 days |
| Middle ear infections | Chronic purulent otitis media | 500 mg twice daily to 750 mg twice daily | 7 -14 days |
| Urinary tract infections | Uncomplicated acute cystitis | 250 mg twice daily to 500 mg twice daily | 3 days |
| A single dose of 500 mg can be used in premenopausal women | |||
| Complicated urinary tract infections | 500 mg twice daily | 7 days | |
| Acute pyelonephritis | 500 mg twice daily to 750 mg twice daily | At least 10 days, in some special clinical cases (such as abscesses) treatment can be extended to more than 21 days | |
| Bacterial prostatitis | 500 mg twice daily to 750 mg twice daily | 2 to 4 weeks (acute) and 4 to 6 weeks (chronic) | |
| Genital infections | Gonococcal urethritis and cervicitis | Single dose 500 mg | 1 day (single dose) |
| Epididymo-orchitis, particularly caused by Neisseria gonorrhoeae | 500 mg twice daily to 750 mg twice daily | At least 14 days | |
| Pelvic inflammatory disease, particularly caused by Neisseria gonorrhoeae | 500 mg twice daily to 750 mg twice daily | At least 14 days | |
| Gastrointestinal tract infections and intra-abdominal infections | Diarrhea caused by bacterial pathogens, particularly Shigella spp., other than Shigella dysenteriae type 1, and severe traveler's diarrhea, as empirical treatment | 500 mg twice daily | 1 day |
| Diarrhea caused by Shigella dysenteriae, type 1 | 500 mg twice daily | 5 days | |
| Diarrhea caused by Vibrio cholerae | 500 mg twice daily | 3 days | |
| Typhoid fever | 500 mg twice daily | 7 days | |
| Intra-abdominal infections caused by gram-negative bacteria | 500 mg twice daily to 750 mg twice daily | From 5 to 14 days | |
| Skin and soft tissue infections caused by gram-negative bacteria | 500 mg twice daily to 750 mg twice daily | From 7 to 14 days | |
| Bone and joint infections | 500 mg twice daily to 750 mg twice daily | Maximum 3 months | |
Fever in patients with neutropenia caused by bacterial infection. Ciprofloxacin should be used concomitantly with appropriate antibacterial agents according to official recommendations. | 500 mg twice daily to 750 mg twice daily | Therapy should be continued throughout the entire period of neutropenia. | |
| Post-exposure prophylaxis and definitive treatment of pulmonary anthrax in individuals who can receive oral treatment, if clinically indicated. Treatment should be initiated as soon as possible after suspected or confirmed exposure. | 500 mg twice daily | 60 days from the date of confirmed contact with Bacillus anthracis | |
Children and adolescents
| Indication | Daily dose, mg | Total duration of treatment (may include initial parenteral administration of ciprofloxacin) |
|---|---|---|
| Bronchopulmonary infections caused by Pseudomonas aeruginosa in patients with cystic fibrosis | 20 mg/kg body weight twice daily with a maximum dose of 750 mg | From 10 to 14 days |
| Complicated urinary tract infections and acute pyelonephritis | From 10 mg/kg body weight twice daily to 20 mg/kg body weight twice daily with a maximum dose of 750 mg | From 10 to 21 days |
Post-exposure prophylaxis and treatment of pulmonary anthrax in patients who can receive oral treatment, if clinically indicated. The drug should be started as soon as possible after suspected or confirmed contact. | 10-15 mg/kg body weight twice daily; maximum single dose 500 mg | 60 days from the date of confirmed contact with Bacillus anthracis |
Elderly patients
Elderly patients
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.