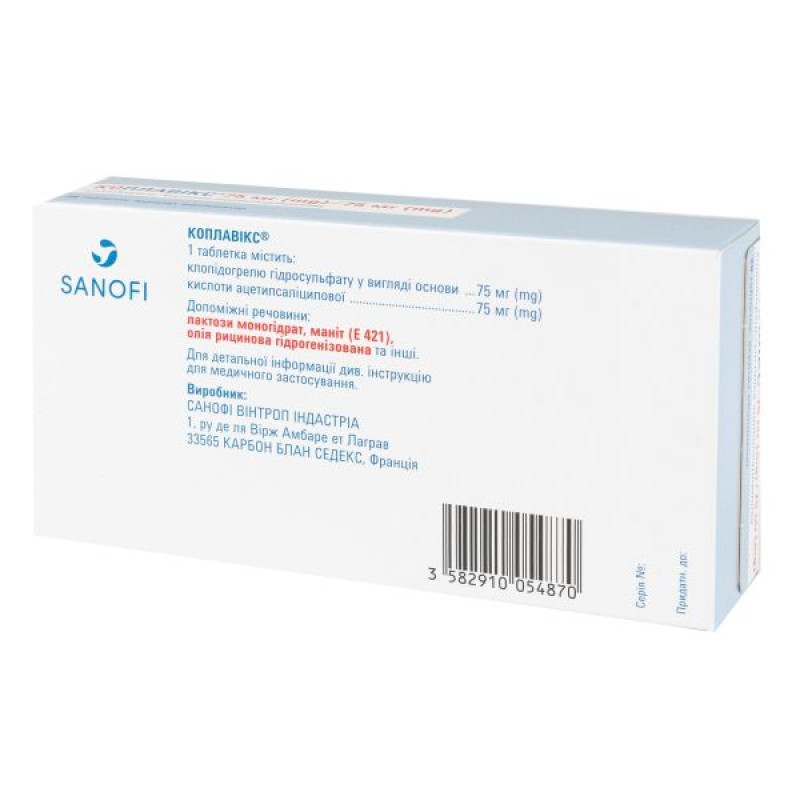
Coplavix film-coated tablets 75 mg + 75 mg blister No. 28

Instructions for use: Koplavix film-coated tablets 75 mg + 75 mg blister No. 28
Composition
active ingredients: clopidogrel, acetylsalicylic acid;
1 tablet contains clopidogrel hydrosulfate as base 75 mg and acetylsalicylic acid 75 mg;
excipients:
clopidogrel layer: mannitol (E 421), macrogol 6000, microcrystalline cellulose (low water content, 90 μm), low-substituted hydroxypropylcellulose, hydrogenated castor oil;
acetylsalicylic acid layer: corn starch, low-substituted hydroxypropyl cellulose, stearic acid, microcrystalline cellulose (with low water content, 90 microns), colloidal anhydrous silicon dioxide;
shell: opadry yellow 32K22174: lactose monohydrate, hypromellose, titanium dioxide (E 171), triacetin, iron oxide yellow (E 172);
Polishing: carnauba wax.
Dosage form
Film-coated tablets.
Main physicochemical properties: slightly convex oval tablets of yellow color, coated, engraved with “С75” on one side and “А75” on the other.
Pharmacotherapeutic group
Antithrombotic agents, platelet aggregation inhibitors, except heparin. ATC code B01A S30.
Pharmacological properties
Pharmacodynamics.
Mechanism of action. Clopidogrel is a prodrug, one of its metabolites is an inhibitor of platelet aggregation. To form the active metabolite that inhibits platelet aggregation, clopidogrel must be metabolized by enzymes of the cytochrome CYP450 system. The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to the P2Y12 receptor on the platelet surface and the subsequent activation of the glycoprotein IIb/IIIa complex by ADP, thereby inhibiting platelet aggregation. Due to the irreversible nature of the binding, platelets that have interacted with clopidogrel remain under its action throughout their lifetime (approximately 7–10 days), and normal platelet function is restored at a rate that corresponds to the rate of platelet renewal. Platelet aggregation induced by agonists other than ADP is also inhibited by blocking the amplification of platelet activation by released ADP.
Since the active metabolite is formed by enzymes of the cytochrome CYP450 system, some of which are polymorphic or inhibited by other drugs, not all patients experience adequate platelet inhibition.
Pharmacodynamic effects. Repeated administration of clopidogrel at a dose of 75 mg per day significantly inhibited ADP-induced platelet aggregation from the first day of administration; this effect gradually increased and reached a constant level with the achievement of a steady state on days 3-7. At steady state, the average level of platelet inhibition observed against a dose of 75 mg per day ranged from 40% to 60%. Platelet aggregation and bleeding time gradually returned to baseline levels over a total of 5 days.
Acetylsalicylic acid inhibits platelet aggregation by irreversible inhibition of prostaglandin cyclooxygenase and thus inhibits the formation of thromboxane A2, which causes platelet aggregation and vasoconstriction. This effect persists throughout the life of the platelet.
Clinical efficacy and safety.
The safety and efficacy of the combination of clopidogrel with ASA were evaluated in three double-blind studies involving more than 61,900 patients: the CURE, CLARITY and COMMIT studies compared the use of the combination of clopidogrel with ASA and ASA monotherapy, both treatment regimens were used in combination with other standard therapy.
The number of patients who reached the primary endpoint (cardiovascular death (CVD), myocardial infarction (MI), or stroke) was 582 (9.3%) in the clopidogrel plus ASA group and 719 (11.4%) in the ASA monotherapy group; the relative risk reduction (RR) was 20% (95% CI 10–28%; p = 0.00009) in the clopidogrel plus ASA group (the relative risk reduction was 17% in patients treated conservatively, 29% in patients treated with percutaneous transluminal coronary angioplasty (PTCA) with or without stenting, and 10% in patients who underwent coronary artery bypass grafting (CABG)). Prevention of new cardiovascular events (primary endpoint) was achieved with relative risk reductions of 22% (CI: 8.6–33.4), 32% (CI: 12.8–46.4), 4% (CI: −26.9–26.7), 6% (CI: −33.5–34.3) and 14% (CI: −31.6–44.2) during the 0–1, 1–3, 3–6, 6–9 and 9–12 months of study, respectively. Thus, after more than 3 months of treatment, the beneficial effect observed in the clopidogrel plus ASA group was not further increased, while the risk of bleeding remained (see section 4.4).
The use of clopidogrel in the CURE study was associated with a reduction in the need for thrombolytic therapy (RR = 43.3%; CI: 24.3–57.5%) and the use of GPIIb/IIIa receptor inhibitors (RR = 18.2%; CI: 6.5–28.3%).
The number of patients who reached the combined primary endpoint (CVD, MI, stroke, or refractory ischemia) was 1035 (16.5%) in the clopidogrel plus ASA group and 1187 (18.8%) in the ASA monotherapy group; the relative risk reduction was 14% (95% CI 6–21%, p = 0.0005) in the clopidogrel plus ASA group. This effect was mainly due to a statistically significant reduction in the incidence of MI (287 (4.6%) in the clopidogrel plus ASA group and 363 (5.8%) in the ASA monotherapy group). There was no effect on the incidence of rehospitalization for unstable angina.
The results obtained in groups of patients with different characteristics (e.g. unstable angina or non-Q-wave MI, low- to high-risk status, diabetes mellitus, need for revascularization, age, gender, etc.) were consistent with the results of the primary analysis. In particular, in a retrospective analysis of 2172 patients (17% of the total CURE population) who underwent stenting (Stent-CURE), clopidogrel compared with placebo demonstrated a significant SVR of 26.2% in favor of clopidogrel for the composite endpoint (CHD, MI, stroke) and a significant SVR of 23.9% for the second composite primary endpoint (CHD, MI, stroke, or refractory ischemia). Moreover, the safety profile of clopidogrel in this subgroup of patients was not of particular concern. Therefore, the results of this subgroup are consistent with the overall results of the study.
In patients with acute ST-segment elevation MI, the safety and efficacy of clopidogrel were evaluated in 2 randomized, placebo-controlled, double-blind studies—CLARITY and COMMIT.
The CLARITY trial enrolled 3491 patients. These patients had an ST-segment elevation MI within the previous 12 hours and were scheduled for thrombolytic therapy. Patients received clopidogrel (loading dose 300 mg, then 75 mg/day, n = 1752) plus ASA or ASA alone (loading dose 150–325 mg, then 75–162 mg/day, n = 1739), a fibrinolytic agent, and, if necessary, heparin. Patients were followed for 30 days. The primary endpoint was the presence of occlusion of the infarct-related artery on angiography before hospital discharge or death or recurrent MI before coronary angiography. In patients who did not undergo angiography, the primary endpoint was death or recurrent MI by day 8 or hospital discharge. The patient population included 19.7% women and 29.2% of patients were ≥65 years of age. A total of 99.7% of patients received fibrinolytics (fibrin-specific 68.7%, fibrin-nonspecific 31.1%), 89.5% heparin, 78.7% beta-blockers, 54.7% ACE inhibitors, and 63% statins.
Fifteen percent (15%) of patients in the clopidogrel plus ASA group and 21.7% in the ASA alone group reached the primary endpoint, representing an absolute reduction of 6.7% and an odds ratio of 36% in favor of clopidogrel (95% CI: 24–47%; p < 0.001), mainly due to a reduction in the incidence of occlusion in infarct-related arteries. This effect was observed in all prespecified subgroups, including those defined by age and sex, infarct location, and type of fibrinolytic or heparin used.
Clopidogrel with ASA significantly reduced the relative risk of all-cause death by 7% (p = 0.029) and the relative risk of the combination of recurrent infarction, stroke, or death by 9% (p = 0.002), representing an absolute reduction of 0.5% and 0.9%, respectively. This effect was observed in patients as early as the first 24 hours, regardless of age, sex, or the use or non-use of fibrinolytics.
Replacement therapy with P2Y12 inhibitors in acute coronary syndrome (ACS).
Switching from a more potent P2Y12 receptor inhibitor to clopidogrel concomitantly with aspirin after an acute phase of ACS was evaluated in two randomized, investigator-sponsored trials (ISS), TOPIC and TROPICAL-ACS, based on clinical outcome data.
The clinical benefits of the more potent P2Y12 receptor inhibitors, ticagrelor and prasugrel, in pivotal trials have been associated with a significant reduction in recurrent ischemic events (including acute and subacute stent thrombosis (ST), myocardial infarction (MI), and urgent revascularization). Despite the consistent benefit in ischemic events over the first year, a more significant reduction in recurrent ischemic events after ACS was observed within the first few days after initiation of treatment. However, retrospective analysis revealed a statistically significant increased risk of bleeding with the more potent P2Y12 receptor inhibitors, which occurred mostly during the maintenance phase one month after ACS. The TOPIC and TROPICAL-ACS trials were designed to investigate the possibility of minimizing bleeding while maintaining treatment efficacy.
TOPIC (Timing Of Platelet Inhibition after acute Coronary syndrome)
This randomized, open-label study enrolled patients with ACS who required PCI (percutaneous coronary intervention). Patients who were taking aspirin and a more potent P2Y12 receptor inhibitor and had no adverse events for one month were assigned to switch to fixed-dose aspirin plus clopidogrel (de-escalation dual antiplatelet therapy (DAPT)) or to continue their current medication regimen (unchanged DAPT).
Overall, the analysis included 645 of 646 patients with ST-segment elevation myocardial infarction and non-ST-segment elevation or unstable angina (de-escalating BP ((n = 322); unchanged BP (n = 323)). 316 patients (98.1%) in the de-escalating BP group and 318 patients (98.5%) in the unchanged BP group were followed up for one year. The median follow-up for both groups was 359 days. The characteristics of the study cohorts were similar for the two groups.
The primary outcome, a composite of cardiovascular death, stroke, urgent revascularization, and BARC (Bleeding Academic Research Consortium) ≥2 hemorrhage at 1 year after ACS, was observed in 43 patients (13.4%) in the deescalation DPA group and 85 patients (26.3%) in the unchanged DPA group (p < 0.01). This statistically significant difference was mainly due to fewer bleeding episodes, with no difference reported in ischemic disease endpoints (p = 0.36), while BARC ≥2 hemorrhage occurred less frequently in the deescalation DPA group (4.0%) compared with the unchanged DPA group (14.9%, p < 0.01). Bleeding episodes, defined as all bleeding events according to the BARC scale, occurred in 30 patients (9.3%) in the deescalated DPA group and in 76 patients (23.5%) in the unchanged DPA group (p < 0.01).
TROPICAL-ACS (Testing Responsiveness to Platelet Inhibition on Chronic Antiplatelet Treatment for Acute Coronary Syndromes)
This randomized, open-label trial enrolled 2,610 patients with biomarker-positive ACS after successful PCI.
Patients were randomized to receive either prasugrel 5 or 10 mg/day (days 0 to 14) (n = 1306) or prasugrel 5 or 10 mg/day (days 0 to 7) followed by clopidogrel 75 mg/day (days 8 to 14) (n = 1304) in combination with ASA (< 100 mg/day). Platelet function tests (AFTs) were performed on day 14. Patients receiving prasugrel monotherapy continued on prasugrel for 11.5 months.
The primary endpoint (composite of CV death, MI, stroke, and BARC ≥2 hemorrhage at 12 months) was met, demonstrating non-inferiority. Ninety-five patients (7%) in the supervised de-escalation group and 118 patients (9%) in the control group (p-value for non-inferiority = 0.0004) experienced an event. Supervised de-escalation did not increase the combined risk of ischemic events (2.5% in the de-escalation group versus 3.2% in the control group; p-value for non-inferiority = 0.0115) or the key secondary endpoint of BARC ≥2 hemorrhage (5% in the de-escalation group versus 6% in the control group (p = 0.23)). The cumulative incidence of all bleeding events (BARC grades 1–5) was 9% (114 events) in the supervised de-escalation group compared with 11% (137 events) in the control group (p = 0.14).
Children: The European Medicines Agency has waived the obligation to submit the results of studies with Coplavix® in all subsets of the paediatric population in the treatment of coronary atherosclerosis (see section 4.2).
Pharmacokinetics.
Clopidogrel.
Absorption: Clopidogrel is rapidly absorbed after single and repeated oral doses of 75 mg/day. The mean peak plasma concentration of unchanged clopidogrel (approximately 2.2–2.5 ng/ml after a single oral dose of 75 mg) is reached approximately 45 minutes after dosing. Absorption is at least 50%, as determined by the amount of clopidogrel metabolites excreted in the urine.
Distribution: In vitro, clopidogrel and the major circulating (inactive) metabolite are reversibly bound to human plasma proteins (98% and 94%, respectively). The binding is unsaturated in vitro over a wide concentration range.
Metabolism. Clopidogrel is extensively metabolized in the liver. In vitro and in vivo, clopidogrel is metabolized by two major metabolic pathways: one via esterases followed by hydrolysis to an inactive metabolite, which is a carboxylic acid derivative (85% of circulating metabolites), and the other via various cytochromes P450. Initially, the metabolism of clopidogrel produces an intermediate metabolite, 2-oxo-clopidogrel. Further metabolism of the intermediate metabolite, 2-oxo-clopidogrel, produces the active metabolite, the thiol derivative of clopidogrel. In vitro, this metabolic pathway is mediated by CYP3A4, CYP2C19, CYP1A2 and CYP2B6 isoenzymes. The active thiol metabolite, which was isolated in vitro, binds rapidly and irreversibly to platelet receptors, thus inhibiting platelet aggregation.
After a single dose of 300 mg clopidogrel, the Cmax of the active metabolite is twice as high as after a 75 mg maintenance dose for 4 days. Cmax is reached approximately 30–60 minutes after administration.
Elimination: Within 120 hours of oral administration of 14C-labeled clopidogrel to humans, approximately 50% was excreted in the urine and approximately 46% in the feces. After a single 75 mg oral dose, the elimination half-life was approximately 6 hours. The elimination half-life of the major circulating (inactive) metabolite was 8 hours after single or repeated dosing.
Pharmacogenetics. CYP2C19 is involved in the formation of both the active metabolite and the intermediate metabolite 2-oxo-clopidogrel. According to the quantitative determination of platelet aggregation ex vivo, the pharmacokinetic parameters and antithrombotic effect of the active metabolite of clopidogrel differ according to the CYP2C19 genotype.
The CYP2C19*1 allele corresponds to fully functional metabolism, while the CYP2C19*2 and CYP2C19*3 alleles correspond to reduced metabolism. The CYP2C19*2 and CYP2C19*3 alleles account for 85% of the reduced function alleles in Caucasians and 99% in Asians. Other alleles associated with reduced metabolism include CYP2C19*4, *5, *6, *7, and *8, but are less common in the general population.
In a crossover study involving 40 healthy volunteers, 10 in each of four CYP2C19 metabolizer groups (ultra-rapid, extensive, intermediate, and poor), pharmacokinetic and antiplatelet responses were evaluated after administration of 300 mg followed by 75 mg/day and 600 mg followed by 150 mg/day for 5 days (steady state). No significant differences in active metabolite concentrations and mean platelet aggregation inhibition (PAI) values were observed between ultra-rapid, extensive, and intermediate metabolizers. In poor metabolizers, active metabolite concentrations were reduced by 63–71% compared with extensive metabolizers. After the 300 mg/75 mg regimen, antiplatelet responses were reduced in poor metabolizers—mean PAO (5 μM ADP) was 24% (at 24 hours) and 37% (at day 5) compared with PAO of 39% (at 24 hours) and 58% (at day 5) in extensive metabolizers and 37% (at 24 hours) and 60% (at day 5) in intermediate metabolizers. When poor metabolizers were on the 600 mg/150 mg regimen, the concentration of the active metabolite was higher than with the 300 mg/75 mg regimen. In addition, the AUC was 32% (at 24 hours) and 61% (at day 5), which was higher than that in poor metabolizers who followed the 300 mg/75 mg regimen and was similar to that in other CYP2C19 metabolizer groups who followed the 300 mg/75 mg daily regimen. The appropriate dosing regimen for this patient group has not been established in clinical studies.
Consistent with the above results, a meta-analysis of 6 studies including steady-state data from 335 participants treated with clopidogrel showed that the concentration of the active metabolite was reduced by 28% in intermediate metabolizers and 72% in poor metabolizers, and the inhibition of platelet aggregation (5 μM ADP) was reduced by 5.9% and 21.4%, respectively, compared with that in extensive metabolizers.
The effect of CYP2C19 genotype on clinical outcomes in patients treated with clopidogrel has not been evaluated in prospective randomized controlled trials. However, a number of retrospective analyses have been conducted to assess this effect in patients treated with clopidogrel for whom genotyping results are available: CURE (n = 2721), CHARISMA (n = 2428), CLARITY-TIMI 28 (n = 227), TRITON-TIMI 38 (n = 1477), and ACTIVE-A (n = 601), as well as a number of published cohort studies.
In the TRITON-TIMI 38 trial and 3 cohort studies (Collet, Sibbing, Giusti), the pooled group of patients with intermediate or poor metabolizers had a higher incidence of cardiovascular events (death, myocardial infarction, and stroke) or stent thrombosis compared with extensive metabolizers.
In the CHARISMA study and one cohort study (Simon), an increased incidence of complications was observed only in poor metabolizers compared with extensive metabolizers.
In the CURE, CLARITY, ACTIVE-A studies and one cohort study (Trenk), no increase in the incidence of complications was observed depending on the metabolizer status.
None of these analyses included sufficient numbers of patients to detect differences in clinical outcomes in poor metabolizers.
Special patient groups: There is no information on the pharmacokinetic parameters of the active metabolite of clopidogrel in these patient groups.
Renal impairment: After repeated administration of clopidogrel 75 mg daily to patients with severe renal disease (creatinine clearance 5 to 15 ml/min), the inhibition of ADP-induced platelet aggregation was less (25%) than in healthy volunteers, but the prolongation of bleeding time was similar to that observed in healthy volunteers receiving 75 mg daily of clopidogrel. In addition, clinical tolerability was satisfactory in all patients.
Hepatic impairment: After repeated administration of clopidogrel 75 mg daily for 10 days in patients with severe hepatic impairment, inhibition of ADP-induced platelet aggregation was similar to that in healthy volunteers. The mean increase in bleeding time was also similar in the two groups.
Race. The prevalence of CYP2C19 alleles that result in moderate or severe reductions in CYP2C19-mediated metabolism varies by race/ethnicity (see Pharmacogenetics). There are limited published data in patients of Asian descent to assess the significance of CYP2C19 genotype on clinical outcomes.
Acetylsalicylic acid (ASA).
Absorption. ASA, which is part of the drug Koplavix®, after absorption is converted to salicylic acid by hydrolysis. The peak level of salicylic acid in the blood plasma is reached within 1 hour after administration. Thus, the level of ASA in the blood plasma is beyond the detection limit 1.5–3 hours after administration of the drug.
Metabolism and elimination. ASA, which is part of the drug Koplavix®, is rapidly converted by hydrolysis into salicylic acid, the half-life of which in the case of ASA doses of 75–100 mg is 0.3–0.4 hours. Salicylic acid is mainly conjugated in the liver, where salicyluric acid, phenolic glucuronide, acyl glucuronide, and a number of secondary metabolites are formed. The plasma half-life of salicylic acid in the drug Koplavix® is approximately 2 hours. The metabolism of salicylates is saturated, the total body clearance decreases in the case of high serum concentrations due to the limited ability of the liver to form both salicyluric acid and phenolic glucuronide. In the case of toxic doses (10–20 g), the half-life from plasma may exceed 20 hours. In the case of high doses of ASA, the elimination of salicylic acid follows zero-order kinetics (i.e., the elimination rate is constant relative to the plasma concentration), with an actual half-life of 6 hours or more. Renal excretion of unchanged active substance depends on the pH of the urine. As the pH of the urine exceeds 6.5, the renal clearance of free salicylate increases from 5 to 80%. After taking therapeutic doses, approximately 10% is observed in the urine in the form of salicylic acid, 75% in the form of salicyluric acid, 10% in the form of phenolic and 5% in the form of acyl glucuronide of salicylic acid.
Given the pharmacokinetic and metabolic characteristics of both compounds, the occurrence of a clinically significant PK interaction is unlikely.
Preclinical safety data.
Clopidogrel.
In preclinical studies in rats and baboons, the most significant changes were observed in the liver. They occurred at doses that were at least 25 times higher than those observed in humans at a dose of 75 mg/day and were due to effects on hepatic enzymes involved in metabolism. No effects on hepatic metabolizing enzymes were observed in humans receiving therapeutic doses of clopidogrel.
At very high doses of clopidogrel, poor gastric tolerability (gastritis, gastric erosions and/or vomiting) was also observed in rats and baboons.
There was no evidence of carcinogenic effects when clopidogrel was administered to mice for 78 weeks and to rats for 104 weeks at doses up to 77 mg/kg/day (which is at least 25 times the concentration observed in humans taking the drug at a clinical dose of 75 mg/day).
Clopidogrel has been tested in a series of in vitro and in vivo genotoxicity studies and has not shown genotoxic activity.
Clopidogrel was found to have no effect on the reproductive function of male and female rats and was not teratogenic in either rats or rabbits. Clopidogrel caused a slight delay in the development of the offspring when administered to lactating female rats. Specific pharmacokinetic studies with radiolabeled clopidogrel have shown that the parent compound or its metabolites are excreted in breast milk. Therefore, a direct (low toxicity) or indirect effect (low palatability) of the drug cannot be excluded.
Acetylsalicylic acid.
Single-dose studies have shown that ASA has low oral toxicity. Repeat-dose toxicity studies have shown that levels up to 200 mg/kg/day are well tolerated in rats; dogs appear to be more sensitive, probably because of the high sensitivity of dogs to the ulcerogenic effects of nonsteroidal anti-inflammatory drugs (NSAIDs). No genotoxicity or clastogenicity concerns have been identified with ASA. Although no formal carcinogenicity studies have been conducted with ASA, it has been shown not to be a tumor-inducing agent.
Reproductive toxicity data show that ASA exhibits teratogenic properties in various laboratory animals.
In animals, administration of a prostaglandin synthesis inhibitor has been shown to result in increased pre- and post-implantation fetal death and embryo-fetal lethality. In addition, an increased incidence of various malformations, including cardiovascular, has been reported in animals treated with a prostaglandin synthesis inhibitor during the period of organogenesis.
Indication
Secondary prevention of atherothrombotic complications in adults already taking clopidogrel and acetylsalicylic acid (ASA). Coplavix® is a fixed-dose combination drug for continued therapy in the following cases:
acute coronary syndrome without ST segment elevation (unstable angina or myocardial infarction without a pathological Q wave on the ECG), including in patients who have undergone stenting during percutaneous coronary intervention;
acute myocardial infarction with ST segment elevation in patients receiving medical treatment and with the possibility of thrombolysis.
Contraindication
Hypersensitivity to the active substances or any excipient.
Severe liver failure.
Hypersensitivity to nonsteroidal anti-inflammatory drugs (NSAIDs), bronchial asthma, rhinitis, nasal polyps. Mastocytosis, when the use of acetylsalicylic acid can cause severe hypersensitivity reactions (including circulatory shock with flushing, hypotension, tachycardia and vomiting).
Severe renal failure (creatinine clearance < 30 ml/min).
Acute peptic ulcers.
Hemorrhagic diathesis.
Severe heart failure.
Simultaneous use of acetylsalicylic acid and methotrexate in doses of 15 mg/week or more (due to increased hematological toxicity of methotrexate - there is a decrease in renal clearance of methotrexate by anti-inflammatory agents and displacement of methotrexate from plasma protein binding by salicylates).
Third trimester of pregnancy (see section "Use during pregnancy or breastfeeding").
Interaction with other medicinal products and other types of interactions
Medicinal products associated with bleeding risk. There is an increased risk of bleeding due to potential additive synergism. Caution should be exercised when prescribing medicinal products associated with bleeding risk (see section 4.4).
Oral anticoagulants. The concomitant use of Coplavix® with oral anticoagulants is not recommended, as it may increase the intensity of bleeding (see section "Special instructions"). Although the administration of clopidogrel at a dose of 75 mg/day in patients receiving long-term warfarin therapy did not change the pharmacokinetics of S-warfarin or the international normalized ratio (INR), the simultaneous use of clopidogrel and warfarin increases the risk of bleeding due to the independent effects of these drugs on hemostasis.
Glycoprotein IIb/IIIa receptor inhibitors. The drug Coplavix® should be used with caution in patients who are simultaneously taking glycoprotein IIb/IIIa receptor inhibitors (see section "Special instructions").
Heparin. In a clinical study conducted in healthy volunteers, clopidogrel did not require a change in the dose of heparin and did not alter the effect of heparin on coagulation. Concomitant use of heparin does not affect the inhibitory effect of clopidogrel on platelet aggregation. A pharmacodynamic interaction is possible between Coplavix® and heparin, which may increase the risk of bleeding. Therefore, concomitant use requires caution (see section "Special instructions").
Thrombolytics. The safety of concomitant use of clopidogrel, fibrin-specific or non-fibrin-specific thrombolytic agents and heparins has been studied in patients with acute myocardial infarction. The incidence of clinically significant bleeding was similar to that observed with concomitant use of thrombolytic agents and heparin with ASA (see section "Adverse reactions"). The safety of concomitant use of Coplavix® and other thrombolytic agents has not been formally established, such a combination requires caution (see section "Adverse reactions").
Nonsteroidal anti-inflammatory drugs (NSAIDs): In a clinical study conducted in healthy volunteers, the concomitant use of clopidogrel and naproxen increased occult gastrointestinal blood loss. Therefore, concomitant use with nonsteroidal anti-inflammatory drugs (NSAIDs), including COX-2 inhibitors, is not recommended (see section 4.4).
The simultaneous use of high doses of salicylates with non-steroidal anti-inflammatory drugs (NSAIDs) (due to a mutual enhancement effect) increases the risk of ulcers and gastrointestinal bleeding.
Experimental data suggest that ibuprofen may inhibit the effects of low-dose aspirin on platelet aggregation when given concomitantly. In one study, a single dose of ibuprofen 400 mg administered 8 hours before or 30 minutes after a dose of immediate-release aspirin (81 mg) was shown to reduce the effect of ASA on thromboxane formation or platelet aggregation. However, the limitations of these data, as well as the statistical uncertainty in extrapolating ex vivo data to clinical cases, suggest that no firm conclusions can be drawn regarding routine use of ibuprofen; it is unlikely that a clinically significant effect will occur with occasional ibuprofen use (see section 5.2).
Selective serotonin reuptake inhibitors (SSRIs). SSRIs affect platelet activation and increase the risk of bleeding, so SSRIs should be used with caution when used concomitantly with clopidogrel.
Metamizole. When used simultaneously with acetylsalicylic acid, metamizole may reduce the effect of ASA on platelet aggregation. In this regard, such a combination should be prescribed with caution to patients taking low doses of ASA in order to achieve a cardioprotective effect.
Other medicines used concomitantly with clopidogrel.
CYP2C19 inducers
Rifampicin is a potent inducer of CYP2C19, leading to both increased levels of the active metabolite of clopidogrel and platelet inhibition, which may in particular increase the risk of bleeding. As a precautionary measure, it is recommended to avoid concomitant use of potent inducers of CYP2C19 (see section 4.4).
CYP2C19 inhibitors
Since the metabolism of clopidogrel to the active metabolite occurs in part by CYP2C19, the use of drugs that inhibit the activity of this enzyme is likely to lead to a decrease in the level of the active metabolite of clopidogrel. Clinical significance
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.