Kineron hard capsules 150 mg blister No. 21
Instructions for Kineron hard capsules 150 mg blister No. 21
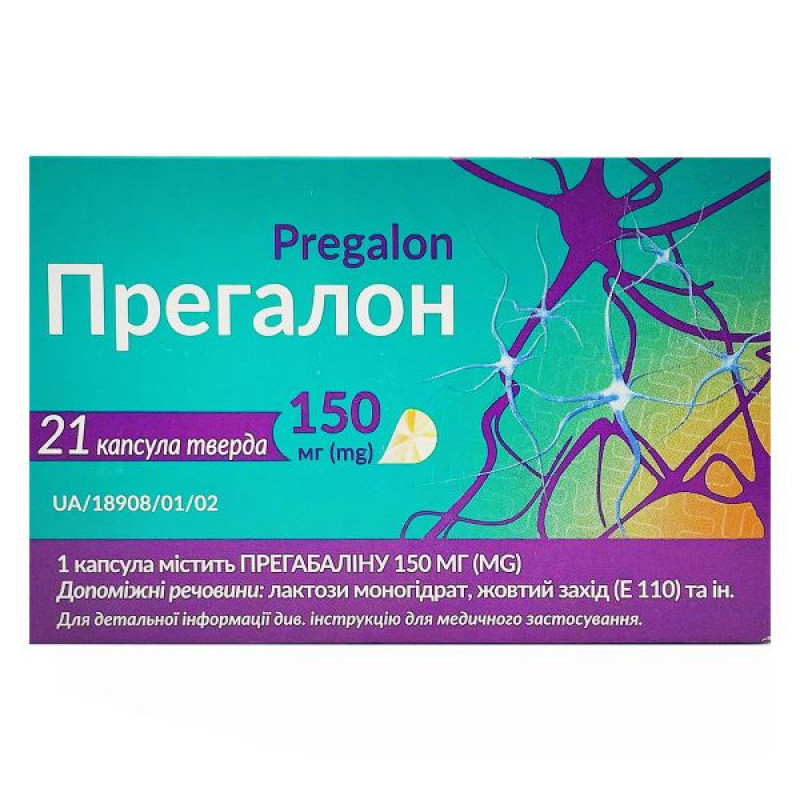
Composition
active ingredient: pregabalin;
1 capsule contains 75 mg, 150 mg or 300 mg of pregabalin;
excipients: lactose monohydrate, corn starch, talc;
capsule shell for 75 mg: gelatin, titanium dioxide (E 171), red iron oxide (E 172), yellow iron oxide (E 172), black iron oxide (E 172);
capsule shell for 150 mg: gelatin, titanium dioxide (E 171), sunset yellow (E 110);
capsule shell for 300 mg: gelatin, titanium dioxide (E 171).
Dosage form
Capsules.
Main physicochemical properties:
hard gelatin capsules of cylindrical shape with an opaque white body and an opaque brown cap (for 75 mg dosage) or an opaque orange cap (for 150 mg dosage) or an opaque white cap (for 300 mg dosage), which are filled with white or almost white powder.
Pharmacotherapeutic group
Antiepileptic drugs, other antiepileptic drugs.
ATX code N03A X16.
Pharmacological properties
Pharmacodynamics
The active substance is pregabalin, which is an analogue of gamma-aminobutyric acid [(S)-3-(aminomethyl)-5-methylhexanoic acid].
Mechanism of action
Pregabalin binds to the auxiliary subunit (a2–d protein) of voltage-gated calcium channels in the central nervous system (CNS).
Clinical efficacy and safety
Neuropathic pain
Studies have shown the drug to be effective in treating diabetic neuropathy, postherpetic neuralgia, and spinal cord injury. The drug's effectiveness in other types of neuropathic pain has not been studied.
Pregabalin has been studied in 10 controlled clinical trials of up to 13 weeks duration with twice daily dosing and in trials of up to 8 weeks duration with three times daily dosing. Overall, the safety and efficacy profiles were similar for the twice and three times daily dosing regimens.
In clinical studies lasting up to 12 weeks in which the drug was used to treat neuropathic pain, a reduction in peripheral and central pain was observed after the first week and was maintained throughout the treatment period.
In controlled clinical trials of peripheral neuropathic pain, 35% of patients treated with pregabalin and 18% of patients treated with placebo achieved a 50% improvement in pain scores. Among patients who did not experience somnolence, this improvement was observed in 33% of patients treated with pregabalin and 18% of patients treated with placebo. Among patients who experienced somnolence, the proportion of patients who responded to treatment was 48% in the pregabalin group and 16% in the placebo group.
In a controlled clinical trial in central neuropathic pain, 22% of patients treated with pregabalin and 7% of patients treated with placebo had a 50% improvement in pain scores.
Epilepsy
Add-on therapy: Pregabalin has been studied in 3 controlled clinical trials of 12 weeks duration with twice-daily or three-times-daily dosing regimens. Overall, the safety and efficacy profiles for the twice-daily and three-times-daily dosing regimens were similar.
A decrease in the frequency of seizures was observed already in the first week.
Children: The efficacy and safety of pregabalin as an adjunctive therapy in epilepsy in children under 12 years of age and adolescents have not been established. Adverse reactions observed in a pharmacokinetic and tolerability study in patients aged 3 months to 16 years (n=65) with partial onset seizures were similar to those seen in adults. Results from a 12-week placebo-controlled study in 295 children aged 4 to 16 years and a 14-day placebo-controlled study in 175 children aged 1 month to 4 years to evaluate the efficacy and safety of pregabalin as adjunctive therapy in partial onset seizures, and a 1-year open-label safety study in 54 children aged 3 months to 16 years with epilepsy, indicate that adverse reactions such as pyrexia and upper respiratory tract infections are more frequently observed in children than in adult patients with epilepsy (see sections 5.2, 5.2 and 4.8).
In a 14-day placebo-controlled study, children (aged 1 month to 4 years) were treated with pregabalin 7 mg/kg/day, pregabalin 14 mg/kg/day, or placebo. The median daily seizure frequency at baseline and final visit was 4.7 and 3.8 for pregabalin 7 mg/kg/day, 5.4 and 1.4 for pregabalin 14 mg/kg/day, and 2.9 and 2.3 for placebo, respectively. Pregabalin 14 mg/kg/day significantly reduced the log-transformed partial-onset seizure frequency compared with placebo (p=0.0223); pregabalin 7 mg/kg/day showed no improvement compared with placebo.
Monotherapy (in newly diagnosed patients). Pregabalin was studied in a single controlled clinical trial of 56 weeks duration with a twice daily dosing regimen. Pregabalin was non-inferior to lamotrigine as assessed at 6 months for the seizure-free endpoint. Pregabalin and lamotrigine were equally safe and well tolerated.
Generalized anxiety disorder
Pregabalin has been studied in six controlled trials of 4–6 weeks duration, one 8-week study in elderly patients, and one long-term relapse prevention trial with a double-blind relapse prevention phase of 6 months duration.
A reduction in symptoms of generalized anxiety disorder according to the Hamilton Anxiety Assessment Scale (HAM-A) was observed as early as week 1.
In controlled clinical trials (4–8 weeks duration), 52% of patients treated with pregabalin and 38% of patients treated with placebo had at least a 50% improvement in HAM-A total score from baseline to endpoint.
In controlled trials, blurred vision was more frequently observed in patients treated with pregabalin than in patients treated with placebo. In most cases, this phenomenon resolved with continued therapy. Ophthalmological examinations (including visual acuity testing, formal visual field testing, and dilated fundus examination) were performed in over 3600 patients in controlled clinical trials. Among these patients, visual acuity deteriorated in 6.5% of patients in the pregabalin group and 4.8% of patients in the placebo group. Visual field changes were observed in 12.4% of patients treated with pregabalin and 11.7% of patients in the placebo group. Fundus changes were observed in 1.7% of patients treated with pregabalin and 2.1% of patients in the placebo group.
Fibromyalgia
The efficacy of pregabalin was established in one 14-week, double-blind, placebo-controlled, multicenter study (F1) and one 6-week, randomized withdrawal study (F2). These studies enrolled patients diagnosed with fibromyalgia based on the American College of Rheumatology criteria (3-month history of widespread pain and pain present in 11 or more of 18 specific tender points). The studies demonstrated a reduction in pain on a visual analog scale. Improvement was additionally demonstrated on the patient's global assessment and on a fibromyalgia impact questionnaire.
Children: A 15-week placebo-controlled study was conducted in 107 children aged 12-17 years with fibromyalgia who received pregabalin at a dose of 75-450 mg/day. The primary efficacy endpoint (change in total pain intensity from baseline to week 15; calculated using an 11-point rating scale) demonstrated a numerically greater improvement in patients treated with pregabalin compared to patients treated with placebo, but this improvement did not reach statistical significance. The most common adverse reactions observed in clinical trials were dizziness, nausea, headache, weight gain, and fatigue. The overall safety profile in adolescents was similar to that in adults with fibromyalgia.
Pharmacokinetics
The steady-state pharmacokinetics of pregabalin were similar in healthy volunteers, patients with epilepsy taking antiepileptic drugs, and patients with chronic pain.
Absorption
Pregabalin is rapidly absorbed in the fasted state and reaches peak plasma concentrations (Cmax) within 1 hour after single or multiple doses. The estimated oral bioavailability of pregabalin is ≥ 90% and is independent of dose. Steady state is reached after 24–48 hours after multiple doses. The rate of absorption of pregabalin is reduced when taken with food, resulting in a decrease in Cmax by approximately 25–30% and a delay in time to peak concentration (tmax) to approximately 2.5 hours. However, taking pregabalin with food had no clinically significant effect on the extent of its absorption.
Distribution
In preclinical studies, pregabalin has been shown to cross the blood-brain barrier in mice, rats, and monkeys. Pregabalin has been shown to cross the placenta in rats and is excreted in the milk of lactating rats. In humans, the volume of distribution of pregabalin after oral administration is approximately 0.56 L/kg. Pregabalin is not bound to plasma proteins.
Pregabalin undergoes minimal metabolism in humans. Following a dose of radiolabeled pregabalin, approximately 98% of the radioactivity was excreted in the urine as unchanged pregabalin. The N-methylated derivative of pregabalin, the major metabolite of the drug detected in urine, accounted for 0.9% of the administered dose. In nonclinical studies, there was no racemization of the S-enantiomer of pregabalin to the R-enantiomer.
Breeding
Pregabalin is eliminated from the systemic circulation unchanged, primarily by the kidneys. The mean elimination half-life of pregabalin is 6.3 hours. The plasma and renal clearance of pregabalin are directly proportional to creatinine clearance (see section "Pharmacokinetics. Renal impairment").
Patients with impaired renal function or patients on hemodialysis require dose adjustment (see section "Method of administration and dosage", Table 1).
Linearity/nonlinearity
The pharmacokinetics of pregabalin are linear over the recommended dose range. Inter-patient variability in the pharmacokinetics of pregabalin is low (as expected from single-dose data). Therefore, routine monitoring of pregabalin plasma concentrations is not required.
Sex
The results of clinical studies indicate that there is no clinically significant effect of gender on pregabalin plasma concentrations.
Kidney failure
Pregabalin clearance is directly proportional to creatinine clearance. In addition, pregabalin is effectively removed from plasma by hemodialysis (after 4 hours of hemodialysis, the concentration of pregabalin in plasma is reduced by approximately 50%). Since the drug is excreted mainly by the kidneys, patients with renal insufficiency should reduce the dose of the drug, and after hemodialysis, an additional dose should be used (see section "Method of administration and dosage", Table 1).
Liver failure
No specific pharmacokinetic studies have been conducted in patients with hepatic impairment. Since pregabalin is not extensively metabolized and is excreted primarily unchanged in the urine, hepatic impairment is unlikely to have a significant effect on pregabalin plasma concentrations.
Children
The pharmacokinetics of pregabalin were evaluated in children with epilepsy (age groups: 1 to 23 months, 2 to 6 years, 7 to 11 years, and 12 to 16 years) at doses of 2.5 mg/kg/day, 5 mg/kg/day, 10 mg/kg/day, and 15 mg/kg/day in a pharmacokinetic and tolerability study.
Following oral administration of pregabalin to children in the fasted state, tmax was generally similar across age groups and ranged from 0.5 hours to 2 hours post-dose.
Pregabalin Cmax and area under the concentration-time curve (AUC) increased linearly with increasing dose in each age group. In children weighing <30 kg, AUC values were 30% lower, due to a 43% increase in weight-adjusted clearance in these patients compared to patients weighing ≥30 kg.
The terminal half-life of pregabalin averaged approximately 3–4 hours in children under 6 years of age and 4–6 hours in children over 7 years of age.
In a population pharmacokinetic analysis, creatinine clearance was shown to be a significant covariate for oral pregabalin clearance and body weight was a significant covariate for the apparent volume of distribution of oral pregabalin, and this relationship was similar in pediatric and adult patients.
The pharmacokinetics of pregabalin in patients under 3 months of age have not been studied (see sections 5.1, 5.2, and 4.8).
Elderly patients
Pregabalin clearance tends to decrease with age. This decrease in oral pregabalin clearance is consistent with the age-related decrease in creatinine clearance. Patients with age-related renal impairment may require a reduction in the dose of pregabalin (see Dosage and Administration, Table 1).
Breastfeeding period
The pharmacokinetics of pregabalin administered at a dose of 150 mg every 12 hours (300 mg daily dose) were evaluated in 10 lactating women for at least 12 weeks postpartum. Breastfeeding had no or negligible effect on the pharmacokinetics of pregabalin. Pregabalin was excreted in breast milk, with mean steady-state concentrations approximately 76% of maternal plasma concentrations. The estimated dose to the breastfed infant (with a mean milk intake of 150 mL/kg/day) from a woman taking pregabalin at a dose of 300 mg/day or a maximum dose of 600 mg/day is 0.31 or 0.62 mg/kg/day, respectively. These estimated doses represent approximately 7% of the total maternal daily dose on a mg/kg basis.
Indication
Neuropathic pain
Pregalon is indicated for the treatment of neuropathic pain of peripheral or central origin in adults.
Epilepsy
Pregalon is indicated in adults as adjunctive treatment for partial seizures with or without secondary generalization.
Generalized anxiety disorder
Pregalon is indicated for the treatment of generalized anxiety disorder in adults.
Fibromyalgia.
Contraindication
Hypersensitivity to the active substance or to any of the excipients listed in the "Composition" section.
Interaction with other medicinal products and other types of interactions
Since pregabalin is excreted primarily unchanged in the urine, undergoes minimal metabolism in humans (≤ 2% of the dose is excreted in the urine as metabolites), does not inhibit the metabolism of other drugs in vitro, and is not bound to plasma proteins, it is unlikely that pregabalin could cause or be the target of pharmacokinetic interactions.
In vivo studies and population pharmacokinetic analysis
Thus, in vivo studies, no clinically significant pharmacokinetic interactions were observed between pregabalin and phenytoin, carbamazepine, valproic acid, lamotrigine, gabapentin, lorazepam, oxycodone or ethanol. Population pharmacokinetic analysis demonstrated that oral antidiabetics, diuretics, insulin, phenobarbital, tiagabine and topiramate had no clinically significant effect on the clearance of pregabalin.
Oral contraceptives, norethisterone and/or ethinyl estradiol
Co-administration of pregabalin with oral contraceptives, norethisterone and/or ethinyl estradiol does not affect the steady-state pharmacokinetics of either drug.
Drugs that affect the CNS
Pregabalin may potentiate the effects of ethanol and lorazepam. During post-marketing surveillance, cases of respiratory failure and coma have been reported in patients taking pregabalin in combination with opioids and/or other CNS depressants. Pregabalin is likely to potentiate the cognitive and gross motor impairments caused by oxycodone.
Interactions in elderly patients
No specific pharmacodynamic interaction studies have been conducted in elderly volunteers. Drug interaction studies have only been conducted in adult patients.
Application features
Patients with diabetes
In accordance with current clinical practice, some patients with diabetes mellitus who gain weight during pregabalin therapy may require dose adjustment of their antidiabetic medicinal products.
Hypersensitivity reactions
Hypersensitivity reactions, including angioedema, have been reported in the post-marketing setting of pregabalin. If symptoms of angioedema such as facial swelling, perioral swelling or upper respiratory tract swelling occur, pregabalin should be discontinued immediately.
Dizziness, drowsiness, loss of consciousness, confusion and mental disorders
Pregabalin has been associated with dizziness and somnolence, which may increase the risk of falls in elderly patients. Loss of consciousness, confusion and mental impairment have also been reported in the post-marketing setting. Therefore, patients should be advised to exercise caution until they are aware of the potential effects of this medicinal product.
Vision disorders
In controlled trials, blurred vision was more frequently observed in patients treated with pregabalin than in patients treated with placebo. In most cases, this phenomenon resolved with continued therapy. In clinical trials in which ophthalmological examinations were performed, the incidence of visual acuity deterioration and visual field changes was higher in patients treated with pregabalin compared to patients in the placebo group; the incidence of fundus changes was higher in patients in the placebo group (see section "Pharmacodynamics").
Post-marketing visual adverse reactions, including vision loss, blurred vision, or other changes in visual acuity, many of which were transient, have also been reported with pregabalin. These visual symptoms may resolve or improve after discontinuation of pregabalin.
Kidney failure
Cases of renal failure have been reported, which were sometimes reversible after discontinuation of pregabalin.
Withdrawal of concomitant antiepileptic drugs
There is currently insufficient data to determine whether concomitant antiepileptic drugs can be withdrawn once seizure control is achieved with the addition of pregabalin to therapy, in order to switch to pregabalin monotherapy.
Withdrawal symptoms
Some patients have experienced withdrawal symptoms after discontinuation of short-term or long-term pregabalin therapy. The following events have been reported: insomnia, headache, nausea, anxiety, diarrhea, flu-like syndrome, nervousness, depression, pain, seizures, hyperhidrosis, and dizziness, which are indicative of physical dependence. This information should be communicated to the patient before starting therapy.
Convulsions, including status epilepticus and grand mal seizures, may occur during pregabalin therapy or shortly after its discontinuation.
Data on pregabalin withdrawal after long-term use indicate that the incidence and severity of withdrawal symptoms may be dose-dependent.
Congestive heart failure has been reported in some patients taking pregabalin since the introduction of pregabalin. This reaction has been observed mainly during the treatment of neuropathic pain with pregabalin in elderly patients with pre-existing cardiovascular disorders. Pregabalin should be used with caution in such patients. This phenomenon may resolve upon discontinuation of pregabalin.
Treatment of neuropathic pain of central origin due to spinal cord injury
During the treatment of central neuropathic pain caused by spinal cord injury, the frequency of adverse reactions in general and CNS adverse reactions, especially drowsiness, was increased. This may be due to the additive effect of concomitant medications (e.g. antispasticity drugs) required for the treatment of this condition. This should be taken into account when prescribing pregabalin for this condition.
Respiratory depression
Cases of severe respiratory depression have been reported with pregabalin. Patients with compromised respiratory function, respiratory or neurological disease, renal impairment, concomitant use of CNS depressants (including opioids), and the elderly may be at increased risk of this serious adverse reaction. Dose adjustment may be necessary for these patients (see Dosage and Administration).
Suicidal thinking and behavior
Suicidal ideation and behavior have been reported in patients treated with antiepileptic drugs for some indications. A meta-analysis of randomized, placebo-controlled trials of antiepileptic drugs also showed a small increased risk of suicidal ideation and behavior. The mechanism of this risk is unknown, and the available data do not exclude the possibility of an increased risk with pregabalin.
Therefore, patients should be monitored closely for signs of suicidal ideation and behavior and appropriate treatment should be considered. Patients (and caregivers of patients) should be advised to seek medical advice if signs of suicidal ideation or behavior emerge.
Lower gastrointestinal dysfunction
Post-marketing reports of lower gastrointestinal events (intestinal obstruction, paralytic ileus, constipation) have been reported when pregabalin was used with medicinal products that may cause constipation, such as opioid analgesics. Precautions should be taken to prevent constipation when pregabalin is used concomitantly with opioids (especially in women and the elderly).
Concomitant use with opioids
Caution is advised when prescribing pregabalin concomitantly with opioids due to the risk of CNS depression (see section 4.5). In a case-control study of opioid users, patients receiving pregabalin concomitantly with an opioid had an increased risk of opioid-related mortality compared with opioids alone (adjusted odds ratio [aOR], 1.68 [95% CI, 1.19–2.36]). This increased risk was observed at low doses of pregabalin (≤ 300 mg, 1.52 aOR [95% CI, 1.04–2.22]), and there was a trend toward increased risk at high doses of pregabalin (> 300 mg, 2.55 aOR [95% CI, 1.24–5.06]).
Misuse, abuse or addiction
Cases of misuse, abuse and dependence have been reported. The drug should be used with caution in patients with a history of substance abuse; patients should be monitored for symptoms of misuse, abuse or dependence on pregabalin (cases of addiction, exceeding the prescribed dose, drug-seeking behavior have been reported).
Encephalopathy
Cases of encephalopathy have been reported, occurring predominantly in patients with underlying conditions that may predispose to encephalopathy.
Lactose intolerance
Pregalon contains lactose. Patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or glucose-galactose malabsorption should not take this medicine.
Use during pregnancy or breastfeeding
Women of childbearing potential/contraception for women and men
Since the potential risk to humans is unknown, women of childbearing potential should use effective contraception.
Pregnancy
There are no adequate data from the use of pregabalin in pregnant women.
Reproductive toxicity has been demonstrated in animal studies. The potential risk to humans is unknown.
Pregalon should not be used during pregnancy unless clearly necessary (when the benefit to the mother clearly outweighs the potential risk to the fetus).
Small amounts of pregabalin have been detected in the milk of nursing women. Nursing women should be advised that breastfeeding is not recommended while taking pregabalin.
Fertility
There are no clinical data on the effect of pregabalin on female fertility.
In a clinical study to investigate the effect of pregabalin on sperm motility, healthy male volunteers were administered pregabalin at a dose of 600 mg per day. No effect on sperm motility was observed after 3 months of treatment.
In a fertility study in female rats, adverse effects on reproductive function were observed. In a fertility study in male rats, adverse effects on reproductive function and development were observed. The clinical relevance of these findings is unknown.
Ability to influence reaction speed when driving vehicles or other mechanisms
Pregabalin may have minor or moderate influence on the ability to drive and use machines. Pregabalin may cause dizziness and drowsiness and thus affect the ability to drive and use machines. Therefore, patients should be advised to refrain from driving, operating complex machinery, or engaging in other potentially hazardous activities until it is known whether this medicinal product affects their ability to perform such activities.
Method of administration and doses
The drug Pregalon is taken regardless of food intake.
This medicine is for oral use only.
Doses
The dose range of the drug can vary within 150–600 mg per day. The daily dose is divided into 2–3 doses.
Neuropathic pain
Pregabalin therapy can be initiated at a dose of 150 mg per day, divided into 2-3 doses. Depending on the individual response and tolerability of the drug by the patient, the dose can be increased to 300 mg per day after 3-7 days, and if necessary - to a maximum dose of 600 mg per day after another 7 days.
Epilepsy
Pregabalin therapy can be initiated at a dose of 150 mg per day, divided into 2-3 doses. Depending on the individual response and tolerability of the drug by the patient, the dose can be increased to 300 mg per day after the first week of treatment. After another week, the dose can be increased to a maximum of 600 mg per day.
Generalized anxiety disorder
The dose, divided into 2-3 doses, may vary between 150-600 mg per day. The need for continued therapy should be reviewed periodically.
Pregabalin therapy can be initiated at a dose of 150 mg per day. Depending on the individual response and tolerability of the drug by the patient, the dose can be increased to 300 mg per day after the first week of treatment. After another week of treatment, the dose can be increased to 450 mg per day. After another week, the dose can be increased to a maximum of 600 mg per day.
Fibromyalgia
The recommended dose for the treatment of fibromyalgia is 300 to 450 mg per day. Treatment should be initiated at 75 mg twice daily (150 mg per day). Depending on efficacy and tolerability, the dose may be increased to 150 mg twice daily (300 mg per day) within one week. For patients for whom 300 mg per day is insufficiently effective, the dose may be increased to 225 mg twice daily (450 mg per day). Although a study has been conducted with a dose of 600 mg per day, there is no evidence that this dose would provide additional benefit; it was also less well tolerated. Given the dose-related adverse reactions, doses above 450 mg per day are not recommended. Since pregabalin is primarily excreted by the kidneys, the dose should be adjusted in patients with impaired renal function.
Pregabalin withdrawal
In accordance with current clinical practice, it is recommended to discontinue pregabalin therapy gradually, over a period of at least one week, regardless of the indication (see sections “Special warnings and precautions for use” and “Adverse reactions”).
Kidney dysfunction
Pregabalin is eliminated from the systemic circulation unchanged, primarily by the kidneys. Since pregabalin clearance is directly proportional to creatinine clearance (see section 5.2), the dose should be reduced in patients with renal impairment as indicated in Table 1, based on creatinine clearance (CLcr), which is determined by the formula:
Pregabalin is effectively removed from plasma by haemodialysis (50% of the drug within 4 hours). For patients on haemodialysis, the daily dose of pregabalin should be adjusted according to renal function. In addition to the daily dose, an additional dose of the drug should be administered immediately after each 4-hour haemodialysis session (see Table 1).
Table 1
Pregabalin dose adjustment according to renal function
| Creatinine clearance (CLcr) (ml/min) | Total daily dose of pregabalin * | Dosage regimen | |
| Starting dose (mg/day) | Maximum dose (mg/day) | ||
| ≥ 60 | 150 | 600 | 2-3 times a day |
| ≥ 30 – | 75 | 300 | 2-3 times a day |
| ≥ 15 – | 25–50 | 150 | 1-2 times a day |
| 25 | 75 | 1 time per day | |
| Additional dose after hemodialysis (mg) | |||
| 25 | 100 | single dose+ |
* The total daily dose (mg/day) should be divided into several doses according to the dosing regimen to obtain a single dose (mg/dose).
+ An additional dose is an additional single dose.
Liver failure
No dose adjustment is necessary for patients with hepatic impairment (see Pharmacokinetics).
Elderly patients
Elderly patients may require a reduction in the dose of pregabalin due to impaired renal function (see section "Special warnings and precautions for use").
Children.
The safety and efficacy of pregabalin in children below the age of 18 years have not been established. Currently available information is provided in the section "Adverse reactions", as well as in the sections "Pharmacodynamics" and "Pharmacokinetics", however, no dosage recommendations can be made for this patient population.
Overdose
After the drug was marketed, the most common adverse reactions reported in pregabalin overdose were drowsiness, confusion, agitation, and restlessness. Seizures have also been reported.
Rare cases of coma have been reported.
Treatment of pregabalin overdose consists of general supportive measures and may include haemodialysis if necessary (see section 4.2, Table 1).
Adverse reactions
In the clinical program for pregabalin, more than 8,900 patients received it, of whom 5,600 were participants in double-blind, placebo-controlled studies. The most frequently reported adverse reactions were dizziness and somnolence. Adverse reactions were usually mild to moderate in severity. In all controlled studies, the discontinuation rate due to adverse reactions was 12% among patients taking pregabalin and 5% among patients taking placebo. The most common adverse reactions leading to discontinuation of study drug in the pregabalin group were dizziness and somnolence.
All adverse reactions that occurred more frequently than placebo and in more than one patient are listed below; these adverse reactions are listed by system organ class and frequency: very common (≥ 1/10); common (≥ 1/100 to < 1/100); reactions are presented in order of decreasing seriousness.
These adverse reactions may also be associated with the course of the underlying disease and/or concomitant use of other medications.
During the treatment of neuropathic pain of central origin caused by spinal cord injury, the frequency of adverse reactions in general and the frequency of adverse reactions from the CNS, especially drowsiness, increased (see section "Special instructions").
Additional adverse reactions reported during post-marketing experience are listed below and are in italics.
Infections and infestations
Common: nasopharyngitis.
Blood and lymphatic system disorders
Uncommon: neutropenia.
On the part of the immune system
Uncommon: hypersensitivity.
Rare: angioedema, allergic reactions, anaphylactoid reactions.
Metabolic disorders, metabolism
Common: increased appetite.
Uncommon: loss of appetite, hypoglycaemia.
From the psyche
Common: euphoric mood, confusion, irritability, disorientation, insomnia, decreased libido.
Uncommon: hallucinations, panic attacks, anxiety, agitation, depression, depressed mood, elevated mood, aggression, mood swings, depersonalisation, fatigue
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.

