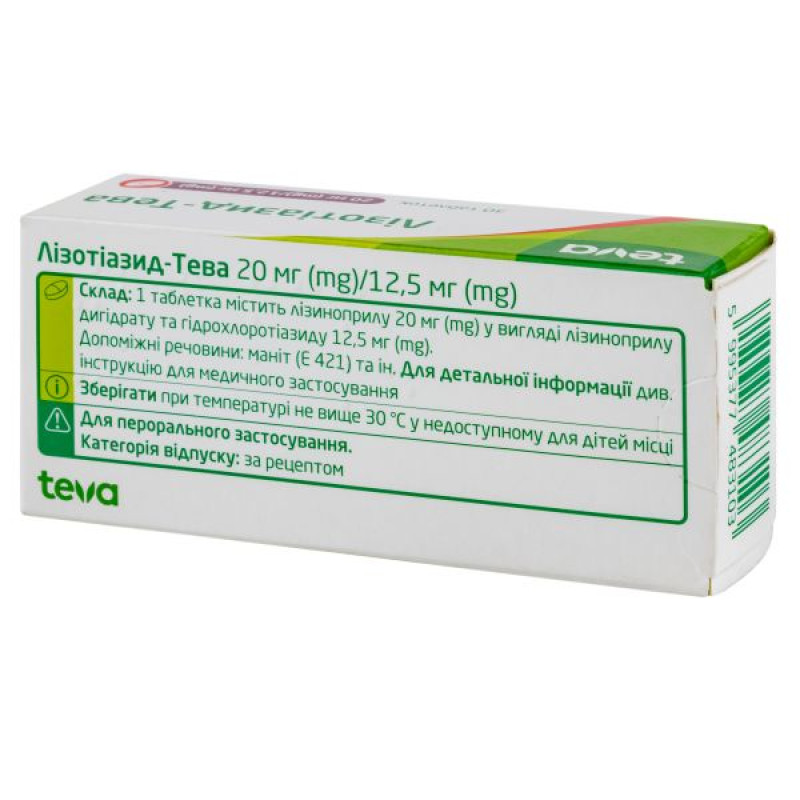
Lisothiazid-Teva tablets 20 mg + 12.5 mg blister No. 30

Pharmacological properties
Pharmacodynamics. Lisinopril and hydrochlorothiazide - an APF inhibitor and a diuretic - have a complementary effect and exhibit an additive antihypertensive effect. APF catalyzes the conversion of angiotensin I to angiotensin II, which has a potent vasoconstrictor effect and stimulates the secretion of aldosterone. The hypotensive effect of lisinopril is associated mainly with inhibition of the renin-angiotensin-aldosterone system with a decrease in the plasma concentration of angiotensin II and aldosterone. Lisinopril has an antihypertensive effect even in patients with low-renin hypertension. APF is similar to kinase II, an enzyme that causes the degradation of bradykinin. It remains unclear whether an increase in the level of bradykinin (a potent vasodilator) plays a role in the therapeutic effect of lisinopril.
Hydrochlorothiazide is a thiazide diuretic and antihypertensive agent that increases plasma renin levels. Hydrochlorothiazide reduces renal reabsorption of electrolytes in the distal loop of Henle and increases the excretion of sodium, chloride, potassium, magnesium, bicarbonate and water. Calcium excretion may be reduced. Concomitant use of lisinopril and hydrochlorothiazide provides a more pronounced hypotensive effect than when these drugs are used in monotherapy. Lisinopril usually reduces the potassium loss caused by hydrochlorothiazide.
Pharmacokinetics. Absorption. Lisinopril: about 25%, with an interindividual variation of 6-60% at the doses studied (5-80 mg). The presence of food in the gastrointestinal tract does not affect the absorption of lisinopril. C max in blood plasma is achieved after 6-8 hours. The effect on blood pressure is noted after 1-2 hours. The maximum effect is achieved after 6 hours and lasts at least 24 hours.
Hydrochlorothiazide: diuretic effect appears after 2 hours. Maximum effect is achieved after 4 hours. Clinically pronounced effect lasts 6-12 hours.
Distribution: Protein binding: Lisinopril is not bound to any plasma protein other than ACE. Elderly patients tend to have higher plasma concentrations of lisinopril due to a reduced volume of distribution than younger patients.
T ½. Lisinopril - 12 hours (after multiple doses). Hydrochlorothiazide - 5.5-15 hours.
Metabolism/Elimination: Both active components are excreted unchanged by the kidneys. After oral administration, about 60% of hydrochlorothiazide is excreted within 24 hours.
Indication
Treatment of hypertension when monotherapy with lisinopril or hydrochlorothiazide is ineffective.
Application
Determining the effective dose of the drug depends on the clinical assessment of the patient's condition.
The usual dose is 1 tablet of 10 mg / 12.5 mg or 20 mg / 12.5 mg once a day. Lisothiazid should be taken daily at approximately the same time. If the expected therapeutic effect cannot be achieved within 2-4 weeks, the dose may be increased to 2 tablets once a day. If the drug is not effective when administered once a day, it is recommended to divide the daily dose into 2 doses. The maximum daily dose of Lisothiazid is 40 mg / 25 mg. The duration of treatment is determined individually, depending on the severity of the disease.
In patients with creatinine clearance of 30 and 80 ml/min, only Lisothiazid 10 mg + 12.5 mg may be used. To avoid symptomatic hypotension in patients taking diuretics, the diuretic should be discontinued 2-3 days before prescribing Lisothiazid.
There is no need for dose adjustment in individuals with hepatic insufficiency.
Taking a fixed combination of lisinopril and hydrochlorothiazide is usually recommended after titrating the doses of the components of the drug separately.
If clinically necessary, direct transfer from monotherapy to a fixed combination of lisinopril and hydrochlorothiazide is possible.
Elderly patients. Elderly patients are more likely to have impaired renal function, so if necessary, dose adjustment should be made for this group of patients. Elderly patients should be carefully examined for objective and subjective symptoms of hypertension.
Contraindication
Hypersensitivity to lisinopril and other ACE inhibitors, hydrochlorothiazide and sulfonamide derivatives or to other components of the drug. Angioedema in history (including after the use of ACE inhibitors, idiopathic and hereditary Quincke's edema). Anuria, severe renal impairment (creatinine clearance 30 ml / min). Severe liver dysfunction. Exacerbation of gout. Simultaneous use of aliskiren-containing drugs in patients with diabetes mellitus or renal impairment (glomerular filtration rate 60 ml / min / 1.73 m2). Mitral or aortic valve stenosis, hypertrophic cardiomyopathy with impaired hemodynamics. Primary hyperaldosteronism. Renal artery stenosis (bilateral or unilateral). Cardiogenic shock. Porphyria. State with unstable hemodynamics after acute myocardial infarction. Use in patients undergoing hemodialysis using high-flux membranes (e.g. an69). Plasma creatinine level 220 μmol/l. Hypokalemia or hypercalcemia resistant to treatment may occur. Refractory hyponatremia. Pregnancy or women planning pregnancy (see Use during pregnancy and lactation).
Side effects
Blood and lymphatic system disorders: bone marrow depression, anemia, thrombocytopenia, leukopenia, neutropenia, agranulocytosis, hemolytic anemia, lymphadenopathy, autoimmune diseases.
Metabolism and nutrition disorders: hypoglycemia, hyperglycemia, hyponatremia.
From the nervous system: dizziness, headache, syncope, paresthesia, taste disturbance, sleep disturbance.
Mental disorders: mood changes, depressive states, confusion.
Cardiovascular: orthostatic effects (including hypotension), patients at high risk may experience myocardial infarction or stroke due to significant hypotension, palpitations, tachycardia, Raynaud's phenomenon, hot flashes.
On the part of the immune system: autoimmune diseases.
From the organs of hearing and balance: vertigo.
Respiratory system: cough, rhinitis, shortness of breath, bronchospasm, sinusitis, allergic alveolitis/eosinophilic pneumonia.
On the part of the digestive system: diarrhea, nausea, vomiting, abdominal pain, dyspepsia, dry mouth, pancreatitis, intestinal angioedema, constipation, bloating.
Hepatobiliary disorders: increased liver enzymes and bilirubin, hepatocellular or cholestatic hepatitis, jaundice and hepatic failure*.
Skin and subcutaneous tissue disorders: rash, pruritus, hypersensitivity/angioedema: angioedema of the face, extremities, lips, tongue, glottis and/or larynx, urticaria, alopecia, psoriasis, increased sweating, pemphigus, toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme, cutaneous pseudolymphoma**.
From the genitourinary system: renal dysfunction, uremia, acute renal failure, oliguria/anuria.
From the reproductive system and mammary glands: impotence, gynecomastia.
Musculoskeletal system: muscle spasms.
On the part of the endocrine system: inappropriate secretion of antidiuretic hormone.
General disorders: fatigue, asthenia, chest pain.
Laboratory tests: increased blood urea, increased plasma creatinine, decreased hemoglobin, decreased hematocrit.
* Isolated cases of hepatitis progressing to hepatic failure have been reported. If jaundice or significant elevations of liver enzymes occur in patients taking the fixed combination of lisinopril/hydrochlorothiazide, the drug should be discontinued and alternative treatment instituted.
** Cases of the development of a symptom complex, which may include one or more of the following reactions, have been reported: fever, vasculitis, myalgia, arthralgia/arthritis, positive antinuclear antibody (ANA) test, increased ESR, eosinophilia and leukocytosis, rash, photosensitivity or other skin manifestations.
Regarding the safety of lisinopril-containing drugs, the following adverse reactions have also been reported: balance disorders, disorientation, smell disorders, glossitis, fainting, muscle spasms, shortness of breath, upper respiratory tract infections, decreased appetite, constipation, skin flushing, proteinuria.
Side effects caused by hydrochlorothiazide
Infections and infestations: sialadenitis.
Blood and lymphatic system disorders: leukopenia, neutropenia/agranulocytosis, thrombocytopenia, aplastic anemia, hemolytic anemia, bone marrow depression.
Metabolism and nutrition disorders: anorexia, hyperglycemia, glycosuria, hyperuricemia, electrolyte imbalance (including hyponatremia, hypokalemia, hypochloremic alkalosis, which can induce hepatic encephalopathy or hepatic coma, hypermagnesemia), increased cholesterol and triglyceride levels, gout, hypercalcemia, decreased glucose tolerance, which can lead to the manifestation of latent diabetes mellitus.
Mental disorders: anxiety, depression, sleep disturbances, disorientation, nervousness, mood swings.
From the nervous system: headache, loss of appetite, paresthesia, dizziness, drowsiness.
On the part of the organ of vision: xanthopsia, temporary visual impairment.
From the organs of hearing and balance: vertigo.
Cardiovascular system: orthostatic hypotension, necrotizing angiitis (vasculitis, cutaneous vasculitis), palpitations, cardiac arrhythmias.
Respiratory system: respiratory disorders (including pneumonia and pulmonary edema).
On the part of the digestive system: irritation of the gastric mucosa, diarrhea, constipation, pancreatitis, dry mouth, thirst, nausea, vomiting.
Hepatobiliary disorders: jaundice (intrahepatic cholestatic jaundice), cholecystitis.
Skin and subcutaneous tissue disorders: photosensitivity, rash, lupus-like reactions, reactivation of cutaneous manifestations of systemic lupus erythematosus, urticaria, anaphylactic reactions, toxic epidermal necrolysis, Stevens-Johnson syndrome.
Musculoskeletal and connective tissue disorders: muscle spasm, muscle weakness, cramps.
From the genitourinary system: renal dysfunction, interstitial nephritis.
From the reproductive system: sexual dysfunction.
General disorders: fever, weakness, pain, shock, exhaustion.
Special instructions
Symptomatic hypotension has been reported rarely in patients with uncomplicated hypertension. The likelihood of hypotension is increased in patients who are dehydrated (e.g., as a result of diuretic therapy, dietary salt restriction, dialysis, diarrhea, or vomiting) and in patients with severe renin-dependent hypertension. In such patients, serum electrolytes should be monitored regularly.
Symptomatic hypotension has been reported in patients with heart failure, whether or not associated with renal insufficiency. This is more common in patients with severe heart failure who are receiving high doses of loop diuretics and who have hyponatremia or functional renal insufficiency. Patients at increased risk of hypotension should be closely monitored during the initial treatment period and during dose titration.
This also applies to patients with coronary heart disease or cerebrovascular disease, in whom a significant decrease in blood pressure can lead to myocardial infarction or cerebral circulation disorder (stroke).
If hypotension occurs, the patient should be placed on his back; if necessary, an intravenous infusion of 0.9% sodium chloride solution should be given. A transient hypotensive reaction is not a contraindication to further doses, which can usually be given without difficulty after restoration of effective blood volume and the transient hypotensive reaction has resolved.
In some patients with heart failure who have normal or low blood pressure, an additional decrease in systemic blood pressure may occur during treatment with lisinopril. This effect is expected and usually does not require discontinuation of lisinopril therapy. If hypotension becomes symptomatic, it may be necessary to reduce the dose or discontinue lisinopril.
In the event of acute myocardial infarction, lisinopril should not be used if treatment with vasodilators may worsen the patient's hemodynamic status.
In case of persistent arterial hypotension (systolic blood pressure 90 mm Hg for more than 1 hour), treatment with the drug should be discontinued.
Aortic and mitral valve stenosis/hypertrophic cardiomyopathy. As with other ACE inhibitors, lisinopril should be used with caution in patients with mitral stenosis or left ventricular outflow obstruction (as in aortic stenosis or hypertrophic cardiomyopathy). If the stenosis is hemodynamically significant, the drug is contraindicated (see Adverse Reactions).
Renal impairment: In patients with heart failure, hypotension occurring at the start of treatment with ACE inhibitors may lead to deterioration of renal function. In such cases, acute renal failure, usually reversible, has been reported.
In some patients with bilateral renal artery stenosis or stenosis of the artery to a solitary kidney, ACE inhibitors have been shown to increase blood urea and plasma creatinine; these effects usually resolve after discontinuation of the drug. The likelihood of such events is particularly high in patients with renal insufficiency.
The presence of renovascular hypertension increases the risk of severe hypotension and renal failure. Treatment of such patients should be initiated under medical supervision with low doses and careful titration. Since diuretics may precipitate the above clinical events, they should be discontinued during the first weeks of treatment with lisinopril and renal function should be closely monitored.
In some patients with hypertension without overt renal vascular disease, the use of lisinopril, especially in the presence of diuretics, causes an increase in blood urea and plasma creatinine; these changes are usually minor and transient. The likelihood of their occurrence is higher in patients with impaired renal function. In such cases, it may be necessary to reduce the dose and / or discontinue diuretics and / or lisinopril.
In case of renal artery stenosis (in particular, in case of bilateral stenosis or stenosis of the artery to a single kidney), taking the drug may cause or worsen renal dysfunction, which may lead to the development of acute renal failure.
Previous diuretic therapy: Diuretics should be discontinued 2-3 days before starting treatment with lisinopril/hydrochlorothiazide. If this is not possible, treatment should be initiated with lisinopril 5 mg monotherapy.
Patients after kidney transplantation: Since there is no experience with the use of lisinopril in patients who have undergone kidney transplantation, the use of lisinopril in such patients is not recommended.
Isolated fatalities have been reported as a result of angioedema of the larynx or tongue. If the swelling extends to the tongue, glottis or larynx, respiratory distress may occur, particularly in patients who have previously undergone surgery on the respiratory tract. In such cases, emergency treatment should be initiated immediately, which may include the administration of adrenaline and/or the maintenance of a patent airway. The patient should be kept under medical supervision until complete and sustained resolution of symptoms.
Patients with a history of angioedema unrelated to ACE inhibitor use may be at increased risk of developing angioedema in response to this class of drugs.
Anaphylactoid reactions during hemodialysis: Anaphylactic reactions have been reported in patients undergoing hemodialysis using high-flux membranes (e.g. AN69) and receiving concomitant ACE inhibitors. These patients should be offered a change of dialysis membrane to a different type of membrane or a different class of antihypertensive drug.
Anaphylactoid reactions during low-density lipoprotein apheresis. Rarely, life-threatening anaphylactic reactions have occurred during low-density lipoprotein apheresis with dextran sulfate in patients receiving ACE inhibitors. Such reactions can be avoided by temporarily discontinuing ACE inhibitor therapy before each apheresis.
Desensitization: Patients receiving ACE inhibitors during desensitization therapy (e.g., to hymenoptera venom) have developed persistent anaphylactoid reactions. These reactions have been avoided in the same patients by temporarily stopping ACE inhibitors, but the reactions have recurred after inadvertent re-administration of the drug.
Hepatic failure. Very rarely, ACE inhibitors have been associated with a syndrome that begins with cholestatic jaundice, progresses rapidly to necrosis, and is sometimes fatal. The mechanism of this syndrome is unknown. Patients who develop jaundice or significantly elevated liver enzymes while taking lisinopril should discontinue the drug and receive appropriate medical attention.
Neutropenia/agranulocytosis. Neutropenia/agranulocytosis, thrombocytopenia and anemia have been reported in patients receiving ACE inhibitors. Neutropenia is rare in patients with normal renal function and in the absence of other complicating factors. Neutropenia and agranulocytosis are reversible after discontinuation of the ACE inhibitor. Lisinopril should be used with extreme caution in patients with collagen vascular disease, patients receiving immunosuppressants, allopurinol or procainamide, and in combination with these factors, especially in the presence of impaired renal function. Some such patients develop severe infections that do not always respond to intensive antibiotic therapy. When using the drug in such patients, it is recommended to periodically monitor the number of leukocytes in the blood and warn the patient about the need to report any signs of infection.
Race: ACE inhibitors may cause more severe angioedema in black patients than in white patients. Also, in this group of patients the hypotensive effect of lisinopril is less pronounced due to the predominance of low-renin fractions.
Lithium: In general, the combination of lithium and lisinopril is not recommended.
Cough: A persistent, nonproductive cough may occur with ACE inhibitors, which resolves after discontinuation of treatment. ACE inhibitor-induced cough should be considered as a possible option in the differential diagnosis of cough.
Surgery/Anesthesia: In patients undergoing surgery or anesthesia with antihypertensive drugs, lisinopril may block the increased formation of angiotensin II under the influence of compensatory renin release. If hypotension resulting from this mechanism is detected, it is necessary to correct the level of BCC.
Hyperkalemia. Some patients taking ACE inhibitors, including lisinopril, have experienced increases in plasma potassium levels. Those at risk for hyperkalemia include patients with renal insufficiency or diabetes mellitus, those taking potassium-sparing diuretics, potassium supplements or potassium-containing salts, and those taking other medicinal products that increase plasma potassium levels (heparin). If the use of these medicinal products during treatment with ACE inhibitors is necessary, regular monitoring of plasma potassium levels is recommended.
Patients with diabetes mellitus: In diabetic patients taking oral antidiabetic agents or insulin, blood glucose levels should be closely monitored during the first month of therapy with ACE inhibitors.
Renal impairment. In patients with renal disease, thiazides may cause azotemia. In patients with renal impairment, a cumulative effect of the drugs is possible. In progressive renal disease characterized by an increase in non-protein nitrogen, the appropriateness of continued therapy should be carefully evaluated and the possibility of discontinuation of diuretic therapy should be considered.
Hepatic impairment: Thiazides should be used with caution in patients with impaired hepatic function or progressive liver disease, since the slightest disturbance of fluid and electrolyte balance in these patients may lead to the development of hepatic coma.
Metabolic and endocrine effects. Thiazide therapy may reduce glucose tolerance. Therefore, in patients with diabetes mellitus, a dose adjustment of insulin or oral antidiabetic (hypoglycemic) drugs may be required. Latent diabetes mellitus may manifest itself during thiazide therapy.
Thiazide therapy may be associated with elevations in cholesterol and triglyceride levels. Some patients taking thiazide diuretics may develop hyperuricemia or manifest gout.
Electrolyte imbalance. As with any diuretic therapy, patients should have their plasma electrolytes monitored periodically. Thiazides, including hydrochlorothiazide, may cause fluid and electrolyte imbalances (hypokalemia, hyponatremia, and hypochloremic alkalosis). Symptoms of fluid and electrolyte imbalance include dry mouth, thirst, weakness, lethargy, drowsiness, restlessness, muscle pain or cramps, muscular weakness, hypotension, oliguria, tachycardia, and gastrointestinal disturbances such as nausea and vomiting.
Although hypokalemia may develop with thiazide diuretics, concomitant use with lisinopril may reduce diuretic-induced hypokalemia. Patients at high risk for hypokalemia include those with cirrhosis of the liver, increased diuresis, inadequate oral replacement of electrolytes, and those receiving corticosteroid or ACTH therapy.
In hot weather, hyponatremia may occur in patients prone to edema. Chloride deficiency is usually mild and does not require treatment.
Thiazides may reduce urinary calcium excretion and cause a slight intermittent increase in plasma calcium levels even in the absence of pronounced disorders of calcium metabolism. Significant hypercalcemia may be a sign of latent hyperparathyroidism, so it is recommended to stop taking thiazide diuretics until parathyroid function is tested. Thiazides may increase renal excretion of magnesium, which may lead to hypomagnesemia.
Doping test: Hydrochlorothiazide may cause a positive doping test.
Other: Hypersensitivity reactions may occur in patients with or without a history of allergic or asthmatic conditions. Exacerbation or reactivation of systemic lupus erythematosus has been reported.
Laboratory parameters. The drug may affect the results of the following laboratory tests: hydrochlorothiazide may reduce the level of protein-bound iodine in the blood plasma (treatment with hydrochlorothiazide should be discontinued before laboratory tests to assess the function of the parathyroid glands) and increase the concentration of free bilirubin in the blood plasma.
Lisinopril/hydrochlorothiazide
Hypotension and fluid and electrolyte imbalance. In some cases, symptomatic hypotension may occur after the first dose of lisinopril/hydrochlorothiazide. The risk of symptomatic hypotension in hypertensive patients is increased in the presence of fluid and electrolyte imbalance (e.g. hypovolemia, hyponatremia, hypochloremic alkalosis, hypomagnesemia or hypokalemia), which may be caused by diuretic therapy, a low-sodium diet, dialysis or intermittent diarrhea or vomiting. In such patients, electrolyte levels in the blood plasma should be monitored regularly.
Initiation of therapy and dose adjustment for patients at increased risk of developing symptomatic hypotension should be carried out with extreme caution.
Treatment of patients with ischemic heart disease or cerebrovascular disorders should be carried out with particular caution, since excessive reduction in blood pressure may cause myocardial infarction or stroke.
In case of acute hypotension, the patient should be placed on his back; if necessary, an intravenous infusion of 0.9% sodium chloride solution should be administered. A transient hypotensive reaction is not a contraindication for further administration of the drug. After restoration of normal blood pressure and effective blood volume, the drug can be continued at a lower dose, or treatment can be continued with one of the two components.
As with other vasodilators, lisinopril/hydrochlorothiazide should be administered with caution to patients with aortic stenosis or hypertrophic cardiomyopathy.
Renal impairment: Thiazides are ineffective in patients with creatinine clearance <30 mL/min (i.e., moderate or severe renal impairment).
In some patients without overt renovascular disease, slight and transient increases in blood urea and plasma creatinine have been observed when lisinopril was administered concomitantly with a diuretic. If such a reaction occurs with lisinopril/hydrochlorothiazide, therapy should be discontinued. Under appropriate circumstances, treatment may be resumed at lower doses, or one of the components may be used alone.
Risk of hypokalemia. When combining an ACE inhibitor with a thiazide diuretic, the possibility of developing hypokalemia cannot be excluded. Therefore, the level of potassium in the blood should be regularly monitored.
Neutropenia/agranulocytosis: The fixed combination of lisinopril and hydrochlorothiazide should be discontinued if neutropenia (neutrophil count <1000/mm3) is detected or suspected.
Dual blockade of the RAAS. The concomitant use of ACE inhibitors, angiotensin II receptor blockers or aliskiren has been reported to increase the risk of hypotension, hyperglycaemia, and renal impairment (including acute renal failure). Therefore, dual blockade of the RAAS through the combined use of ACE inhibitors, angiotensin II receptor blockers or aliskiren is not recommended.
If dual blockade therapy is necessary, it should be carried out under specialist supervision and with regular monitoring of renal function, electrolyte levels and blood pressure. The concomitant use of ACE inhibitors and angiotensin II receptor blockers is not recommended in patients with diabetic nephropathy.
Use during pregnancy or breastfeeding. Pregnancy. The drug should not be used in women planning pregnancy. If pregnancy is confirmed during treatment with the drug, its use should be discontinued immediately and, if necessary, replaced with another drug approved for use in pregnant women.
Breastfeeding
ACE inhibitors: Because no data are available regarding the use of lisinopril/hydrochlorothiazide during breast-feeding, lisinopril/hydrochlorothiazide is not recommended and alternative treatments with better established safety profiles during breastfeeding are preferable, especially while nursing a newborn or preterm infant.
Hydrochlorothiazide. Hydrochlorothiazide is excreted in small amounts in breast milk. Thiazides in high doses, which cause intense diuresis, may suppress milk production. It is not recommended to use lisinopril / hydrochlorothiazide during breastfeeding. If lisinopril / hydrochlorothiazide is used during breastfeeding, its dose should be as low as possible.
Thus, the drug is contraindicated for use during breastfeeding.
Children: The safety and efficacy of lisinopril/hydrochlorothiazide in children have not been established and should not be used in this age group.
Ability to influence the reaction rate when driving vehicles or operating machinery. It should be borne in mind that while taking lisinopril, the ability to drive vehicles or operate potentially dangerous machinery may be impaired due to possible dizziness and fatigue.
Interactions
Dual blockade of the RAAS. It has been demonstrated that dual blockade of the RAAS with the simultaneous use of ACE inhibitors, angiotensin II receptor antagonists or aliskiren is characterized by a higher frequency of adverse reactions, such as arterial hypotension, hyperglycemia, impaired renal function (including AKI), compared with the use of monotherapy.
lisinopril
Diuretics: When initiating the combination of lisinopril with diuretics, patients may occasionally experience excessive decreases in blood pressure. The risk of symptomatic hypotension with lisinopril may be reduced by discontinuing diuretic therapy before initiating lisinopril therapy.
NSAIDs, including acetylsalicylic acid ≥3 g/day. Long-term use of NSAIDs may reduce the antihypertensive effect of ACE inhibitors, cause an increase in plasma potassium levels, and impair renal function. These effects are usually reversible. Acute renal failure may rarely develop, especially in patients at risk, such as the elderly and those with dehydration.
Other antihypertensive drugs. Concomitant use of these drugs may increase the hypotensive effect of lisinopril. Concomitant use with nitroglycerin and other nitrates or other vasodilators may further reduce blood pressure.
Tricyclic antidepressants/neuroleptics/anesthetics. Concomitant use of certain anesthetic medications, tricyclic antidepressants, and neuroleptics with ACE inhibitors may further lead to a decrease in blood pressure.
Sympathomimetic drugs: Sympathomimetic drugs may reduce the antihypertensive effect of ACE inhibitors.
Acetylsalicylic acid, thrombolytics, β-adrenergic blockers, nitrates. Lisinopril can be used concomitantly with acetylsalicylic acid (in cardiological doses), thrombolytics, β-adrenergic blockers and/or nitrates.
Allopurinol: Concomitant use of ACE inhibitors with allopurinol increases the risk of renal failure and may lead to an increased risk of leukopenia.
Cyclosporine: Concomitant use of ACE inhibitors and cyclosporine increases the risk of renal failure and hyperkalemia.
Lovastatin. Concomitant use of ACE inhibitors and lovastatin increases the risk of hyperkalemia.
Procainamide, cytostatics or immunosuppressive drugs. Concomitant use of these drugs with ACE inhibitors may lead to an increased risk of leukopenia.
Hemodialysis: Lisinopril/hydrochlorothiazide is not indicated in patients requiring dialysis because a high incidence of anaphylactoid reactions has been reported in patients dialyzed with high-flux membranes (e.g. AN69) and concomitantly treated with ACE inhibitors.
Gold: Nitritoid reactions (symptoms of vasodilation including flushing, nausea, dizziness, hypotension, which may be very severe) following injection of a gold preparation (e.g. sodium aurothiomalate) have been reported more frequently in patients treated with ACE inhibitors.
Lithium: The combination of lithium and lisinopril is not recommended.
Hydrochlorothiazide
Amphotericin B (for parenteral use), carbenoxolone, corticosteroids, corticotropin (ACTH), or stimulant laxatives. Concomitant use with hydrochlorothiazide may cause electrolyte imbalance, particularly hypokalemia.
Calcium salts. When used together with thiazides, an increase in plasma calcium levels may occur as a result of a decrease in its excretion.
Cardiac glycosides. Increased risk of digitalis intoxication in the presence of thiazide-induced hypokalemia.
Cholestyramine and colestipol resins. Concomitant use with hydrochlorothiazide may reduce or delay the absorption of hydrochlorothiazide. Therefore, sulfonamide diuretics should be taken at least 1 hour before or 4-6 hours after taking these drugs.
Non-depolarizing muscle relaxants (tubocurarine chloride). The effect of these drugs may be enhanced by hydrochlorothiazide.
Drugs that induce paroxysmal ventricular tachycardia pirouette: Due to the risk of hypokalemia, special caution should be exercised when hydrochlorothiazide is used concomitantly with drugs that are associated with paroxysmal ventricular tachycardia pirouette, such as some antipsychotics and other drugs.
Sotalol: Thiazide-induced hypokalemia may increase the risk of sotalol-induced arrhythmias.
NSAIDs: Concomitant use with hydrochlorothiazide may weaken the hypotensive effect of thiazide diuretics.
Ethanol / barbiturate group drugs / narcotic analgesics. Orthostatic hypotension is possible.
Antidiabetic drugs (oral agents and insulins): Dose adjustment of antidiabetic drugs may be required.
Gout medications. Dosage adjustment of gout medications may be necessary as hydrochlorothiazide may increase plasma uric acid levels. Dose adjustment of probenecid or sulfinpyrazone may be necessary. Concomitant use of thiazide diuretics may increase the incidence of hypersensitivity reactions to allopurinol.
Hydrochlorothiazide may reduce the plasma levels of iodine bound to
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.