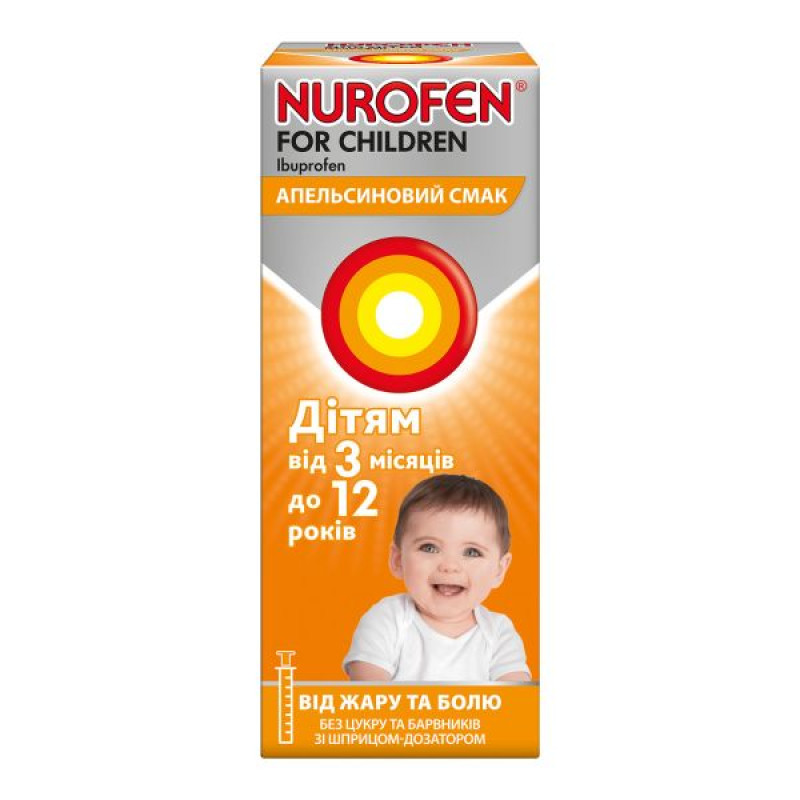
Nurofen for children oral suspension 100 mg/5 ml bottle with orange flavor 100 ml
Instructions Nurofen for children oral suspension 100 mg/5 ml bottle with orange flavor 100 ml
Composition
active ingredient: ibuprofen;
5 ml of suspension contains 100 mg of ibuprofen;
excipients: liquid maltitol; citric acid, monohydrate; sodium citrate; sodium chloride; sodium saccharin; domiphen bromide; polysorbate 80; xanthan gum; orange flavoring 2M16014; glycerin; purified water.
Dosage form
Oral suspension with orange flavor.
Main physicochemical properties: white or almost white suspension with an orange odor.
Pharmacotherapeutic group
Nonsteroidal anti-inflammatory and antirheumatic drugs. Propionic acid derivatives.
ATX code M01A E01.
Pharmacological properties
Pharmacodynamics
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID), a propionic acid derivative, which has been shown to act by inhibiting prostaglandin synthesis. In humans, ibuprofen reduces inflammatory pain, swelling, and fever. Ibuprofen has analgesic, antipyretic, and anti-inflammatory effects. The onset of analgesic and antipyretic effects of ibuprofen has been shown to occur within 30 minutes. In addition, ibuprofen reversibly inhibits platelet aggregation.
Experimental data suggest that ibuprofen may inhibit the effect of low-dose acetylsalicylic acid (aspirin) on platelet aggregation when these drugs are used concomitantly. In a study in which a single dose of ibuprofen 400 mg was taken within 8 hours before or within 30 minutes after immediate-release aspirin (81 mg), a reduced effect of acetylsalicylic acid on thromboxane formation or platelet aggregation was observed. However, the limitations of these data and the uncertainty regarding the extrapolation of ex vivo data to the clinical picture do not allow for firm conclusions to be drawn regarding the routine use of ibuprofen. Therefore, such clinically significant effects are considered unlikely with non-routine use of ibuprofen.
Pharmacokinetics
Ibuprofen is rapidly absorbed after administration and is rapidly distributed throughout the body. Excretion is rapid and complete and occurs via the kidneys.
Maximum plasma concentrations are reached 45 minutes after oral administration in the fasted state. When administered with food, peak levels are observed after 1-2 hours. This time may vary for different dosage forms.
The half-life is approximately 2 hours.
In limited studies, ibuprofen has been found in breast milk at very low concentrations.
Indication
Symptomatic treatment of fever and pain of various origins in children aged 3 months to 12 years with a body weight of at least 5 kg (including fever after immunization, acute respiratory viral infections, influenza, teething pain, pain after tooth extraction, toothache, headache, sore throat, pain from sprains and other types of pain, including inflammatory genesis).
Contraindication
Hypersensitivity to ibuprofen or to any of the excipients of the drug.
History of hypersensitivity reactions (e.g. bronchospasm, bronchial asthma, rhinitis, angioedema or urticaria) after taking acetylsalicylic acid (aspirin) or other non-steroidal anti-inflammatory drugs (NSAIDs).
Active or recurrent gastric ulcer/bleeding (two or more severe episodes of confirmed ulcer or bleeding).
History of gastrointestinal bleeding or perforation associated with NSAID use.
Severe liver failure, severe kidney failure or severe heart failure.
Severe dehydration (caused by vomiting, diarrhea, or insufficient fluid intake).
The last trimester of pregnancy.
Cerebrovascular or other bleeding.
Violation of hematopoiesis of unknown etiology or blood clotting.
Hereditary fructose intolerance.
Interaction with other medicinal products and other types of interactions
Ibuprofen, like other NSAIDs, should not be used in combination with:
- acetylsalicylic acid (aspirin), as this may increase the risk of adverse reactions, unless aspirin (dose not exceeding 75 mg per day) has been prescribed by a doctor. Experimental data suggest that ibuprofen may inhibit the antiplatelet effect of low-dose aspirin when used concomitantly. However, the limited data and uncertainty regarding the extrapolation of ex vivo data to the clinical picture do not allow for firm conclusions regarding the systematic use of ibuprofen. Therefore, such clinically significant effects are considered unlikely with non-systematic use of ibuprofen;
- other NSAIDs, including selective cyclooxygenase-2 inhibitors. The simultaneous use of two or more NSAIDs should be avoided, as this may increase the risk of side effects.
Ibuprofen should be used with caution in combination with the following drugs:
Antihypertensives (ACE inhibitors, beta-blockers and angiotensin II antagonists) and diuretics: NSAIDs may reduce the effect of these drugs. In some patients with impaired renal function (e.g. dehydrated patients or elderly patients with compromised renal function), the concomitant use of ACE inhibitors, beta-blockers or angiotensin II antagonists and cyclooxygenase inhibitors may lead to further deterioration of renal function, including possible acute renal failure, which is usually reversible. Therefore, such a combination should be used with caution, especially in the elderly. Patients should be adequately hydrated and liver function should be monitored after initiation of concomitant therapy and periodically thereafter. Diuretics may increase the risk of nephrotoxicity of NSAIDs.
corticosteroids: increased risk of ulcers and bleeding in the gastrointestinal tract;
Antiplatelet agents and selective serotonin reuptake inhibitors: increased risk of gastrointestinal bleeding;
Cardiac glycosides: e.g. digoxin: NSAIDs may exacerbate cardiac dysfunction, reduce glomerular filtration rate and increase plasma glycoside levels. Concomitant use of ibuprofen with digoxin may increase serum levels of these drugs. With proper use (maximum 4 days), monitoring of serum digoxin levels is usually not required;
Lithium: There is evidence of a potential increase in plasma lithium levels. With proper use (maximum 4 days), monitoring of serum lithium levels is usually not required;
Methotrexate: there is a possibility of increasing the levels of methotrexate in the blood plasma. The use of ibuprofen within 24 hours before or after the administration of methotrexate may lead to an increase in the concentration of methotrexate and an increase in its toxic effect;
cyclosporine: increased risk of nephrotoxicity;
Mifepristone: NSAIDs should not be used earlier than 8-12 days after mifepristone administration, as they may reduce its effectiveness;
Tacrolimus: possible increased risk of nephrotoxicity with concomitant use of NSAIDs with tacrolimus;
Zidovudine: Increased risk of hematological toxicity with concomitant use of zidovudine and NSAIDs. There is evidence of an increased risk of hemarthrosis and hematoma in HIV-infected patients with hemophilia when treated concomitantly with zidovudine and ibuprofen.
Quinolone antibiotics: Animal data suggest that NSAIDs may increase the risk of seizures associated with the use of quinolone antibiotics. Patients taking NSAIDs and quinolones may be at increased risk of developing seizures.
Sulfonylurea drugs: possible potentiation of the effect. Clinical studies have shown an interaction between NSAIDs and antidiabetic drugs (sulfonylureas). Although no interactions between ibuprofen and sulfonylureas have been described to date, it is recommended to monitor blood glucose levels as a precautionary measure when these drugs are used concomitantly;
Phenytoin: serum levels of these drugs may increase. With proper use (maximum 4 days), monitoring of phenytoin serum levels is usually not required;
Probenecid and sulfinpyrazone: medicines containing probenecid or sulfinpyrazone may delay the elimination of ibuprofen;
Potassium-sparing diuretics: simultaneous use of ibuprofen and potassium-sparing diuretics may lead to hyperkalemia (it is recommended to monitor serum potassium levels);
CYP2C9 inhibitors: Concomitant use of ibuprofen with CYP2C9 inhibitors may increase the exposure of ibuprofen (CYP2C9 substrate). A study with voriconazole and fluconazole (CYP2C9 inhibitors) has shown an increase in the exposure of S (+)-ibuprofen by approximately 80-100%.
When ibuprofen is used concomitantly with strong CYP2C9 inhibitors, a reduction in ibuprofen doses is recommended, especially when high doses of ibuprofen are used together with voriconazole or fluconazole.
Application features
Side effects associated with ibuprofen can be minimized by using the lowest effective dose necessary to treat symptoms for the shortest period of time.
Elderly patients have an increased frequency of adverse reactions to NSAIDs, especially gastrointestinal bleeding and perforation, which can be fatal. Elderly patients are at increased risk of adverse reactions. Long-term use of NSAIDs in the elderly is not recommended. If long-term therapy is necessary, patients should be regularly monitored.
Caution should be exercised in patients with the following conditions:
- systemic lupus erythematosus, as well as mixed connective tissue disease - due to an increased risk of aseptic meningitis;
- congenital disorder of porphyrin metabolism, such as acute concomitant porphyria;
- history of hypertension and/or heart failure, as fluid retention and edema have been reported in association with NSAID therapy;
- renal failure - due to the possibility of deterioration of kidney function;
- liver dysfunction;
- immediately after extensive surgical interventions;
- hay fever, nasal polyps or chronic obstructive airways disease due to an increased risk of allergic reactions. These include asthma attacks (so-called analgesic asthma), angioedema or urticaria;
- patients with a history of allergic reactions to other substances, due to an increased risk of hypersensitivity reactions to ibuprofen.
Effects on the respiratory system.
Bronchospasm may occur in patients who suffer from bronchial asthma or allergic diseases or have a history of these diseases.
Other NSAIDs.
The concomitant use of ibuprofen with other NSAIDs, including selective cyclooxygenase-2 inhibitors, should be avoided as this increases the risk of adverse reactions.
Systemic lupus erythematosus and mixed connective tissue disease.
Ibuprofen should be used with caution in systemic lupus erythematosus and mixed connective tissue disease due to an increased risk of aseptic meningitis.
Effects on the cardiovascular and cerebrovascular systems.
Patients with a history of hypertension and/or heart failure should start treatment with caution (consultation with a doctor is necessary), since cases of fluid retention, hypertension and edema have been reported with ibuprofen therapy, as with other NSAIDs.
Clinical trial data and epidemiological data suggest that the use of ibuprofen, especially at high doses (2400 mg/day) and in long-term treatment, may be associated with a small increased risk of arterial thrombotic events (e.g. myocardial infarction or stroke). Overall, epidemiological studies do not suggest that low doses of ibuprofen (e.g. ≤1200 mg/day) are associated with an increased risk of myocardial infarction.
Effect on the kidneys.
In general, the habitual use of analgesics, especially combinations of different analgesics, can lead to long-term kidney damage with the risk of kidney failure (analgesic nephropathy).
Caution should be exercised in patients with renal insufficiency due to the possibility of worsening renal function.
There is a risk of kidney failure in children and adolescents with dehydration.
Effect on the liver.
Liver dysfunction.
Effect on the gastrointestinal tract.
NSAIDs should be used with caution in patients with a history of gastrointestinal diseases (ulcerative colitis, Crohn's disease) as their condition may be exacerbated. Such patients should seek medical advice.
There are reports of cases of gastrointestinal bleeding, perforation, ulceration, which can be fatal, occurring at any stage of treatment with NSAIDs, regardless of the presence of warning symptoms or the presence of severe gastrointestinal disorders in history.
The risk of gastrointestinal bleeding, ulceration or perforation increases with increasing doses of NSAIDs, in the presence of a history of peptic ulcer disease, especially complicated by bleeding or perforation, and in elderly patients. These patients should start treatment with the lowest dose. In such patients, as well as in patients who require concomitant use of low doses of acetylsalicylic acid or other drugs that may increase the risk from the gastrointestinal tract, combination therapy with protective drugs (e.g. misoprostol or proton pump inhibitors) is recommended.
Patients with a history of gastrointestinal toxicity, especially the elderly, should be informed of any unusual gastrointestinal symptoms (especially gastrointestinal bleeding), particularly at the beginning of treatment.
Caution should be exercised when treating patients who are concomitantly taking medications that may increase the risk of ulceration or bleeding, such as oral corticosteroids, anticoagulants (e.g. warfarin), selective serotonin reuptake inhibitors or antiplatelet agents (e.g. acetylsalicylic acid).
In the event of gastrointestinal bleeding or ulceration in patients receiving ibuprofen, treatment should be discontinued immediately.
Impaired fertility in women.
There is limited evidence that cyclooxygenase/prostaglandin synthesis inhibitors may impair fertility in women by affecting ovulation. This is reversible upon discontinuation of therapy.
Severe skin reactions.
Rare serious skin reactions, which can be fatal, including exfoliative dermatitis, Stevens-Johnson syndrome and toxic epidermal necrolysis, have been reported in association with the use of non-steroidal anti-inflammatory drugs (NSAIDs) (see section 4.8).
Ibuprofen should be discontinued at the first signs and symptoms of skin lesions, such as skin rashes, mucosal lesions, or any other signs of hypersensitivity.
In exceptional cases, chickenpox can cause severe skin and soft tissue infections. At this time, the effect of NSAIDs on the worsening of these infections cannot be excluded, therefore it is recommended to avoid the use of ibuprofen in case of chickenpox.
Masking the symptoms of underlying infections.
This medicine may mask the symptoms of an infectious disease, which may delay the initiation of appropriate treatment and thereby complicate the course of the disease. This has been observed in bacterial community-acquired pneumonia and bacterial complications of varicella. When the medicine is used for fever or for pain relief in an infection, monitoring for the infectious disease is recommended. In the context of treatment outside a medical institution, the patient should consult a doctor if symptoms persist or worsen.
Severe acute hypersensitivity reactions (e.g. anaphylactic shock) have been observed very rarely. At the first signs of a hypersensitivity reaction after taking ibuprofen, therapy should be discontinued and a doctor should be consulted immediately.
Ibuprofen may temporarily inhibit platelet aggregation. Therefore, it is recommended to carefully monitor the condition of patients with blood clotting disorders.
With prolonged use of ibuprofen, liver function tests, kidney function, and hematological function/blood count should be checked regularly.
Prolonged use of any painkiller for headache may worsen this condition. In such cases, a doctor should be consulted and treatment should be discontinued. The possibility of medication overuse headache should be considered in patients who suffer from frequent or daily headaches despite (or because of) regular use of headache medications.
The concomitant use of alcohol and NSAIDs may increase adverse reactions associated with the active substance, especially those affecting the gastrointestinal tract or central nervous system.
NSAIDs can mask symptoms of infection and fever.
This medicinal product contains liquid maltitol. It should not be administered to patients with rare hereditary problems of fructose intolerance. Due to the presence of liquid maltitol, this medicinal product may have a mild laxative effect.
This medicinal product contains 27.75 mg sodium per 15 ml suspension (equivalent to 1.85 mg sodium per 1 ml suspension). This should be taken into consideration by patients on a controlled sodium diet.
If you are an adult, talk to your doctor or pharmacist before taking this medicine if: you are pregnant, you are trying to get pregnant, you are of childbearing age, you smoke.
Use during pregnancy or breastfeeding
The drug is used in children under 12 years of age.
Pregnancy.
Inhibition of prostaglandin synthesis may adversely affect pregnancy and/or embryonal/fetal development. Epidemiological data suggest an increased risk of miscarriage, congenital heart defects and gastroschisis following exposure to prostaglandin synthesis inhibitors in early pregnancy. The risk is thought to increase with dose and duration of therapy. The absolute risk of cardiovascular malformations increased from less than 1% to approximately 1.5%.
From the 20th week of pregnancy onwards, ibuprofen may cause oligohydramnios due to fetal renal dysfunction. This may occur shortly after initiation of treatment and is usually reversible after discontinuation of treatment. In addition, there have been reports of narrowing of the ductus arteriosus following treatment in the second trimester of pregnancy, most of which resolved after discontinuation of treatment. Therefore, ibuprofen should not be given during the first and second trimesters of pregnancy unless clearly necessary. If ibuprofen is used by a woman attempting to conceive or during the first and second trimesters of pregnancy, the dose should be kept as low and the duration of treatment as short as possible. Antenatal monitoring for oligohydramnios and narrowing of the ductus arteriosus should be considered after exposure to ibuprofen for several days from the 20th week of gestation onwards. Ibuprofen should be discontinued if oligohydramnios or narrowing of the ductus arteriosus is detected.
During the third trimester of pregnancy, all prostaglandin synthesis inhibitors may pose risks:
Risks to the fetus:
– cardiopulmonary toxicity (premature narrowing/closure of the ductus arteriosus and pulmonary hypertension);
– renal dysfunction (see above);
Risks for the mother at the end of pregnancy and for the newborn:
– possible prolongation of bleeding time, anti-aggregation effect, which can occur even at very low doses;
– suppression of uterine contractions, leading to delayed or prolonged labor.
Breastfeeding. Ibuprofen and its metabolites are excreted in breast milk in low concentrations. There are currently no known adverse effects on the infant, so for short-term treatment of pain and fever at recommended doses, it is usually not necessary to interrupt breastfeeding.
Fertility.
There is some evidence that drugs that inhibit cyclooxygenase/prostaglandin synthesis may impair female fertility by affecting ovulation. This effect is reversible upon discontinuation of treatment.
Therefore, the use of ibuprofen is not recommended for women who have difficulty becoming pregnant.
Ability to influence reaction speed when driving or using other mechanisms
The drug is used in children under 12 years of age. When used in accordance with the recommended doses and duration of treatment, the drug is not expected to affect the ability to drive or operate other mechanisms.
Method of administration and doses
The lowest effective dose should be used for the shortest time necessary to relieve symptoms (see section "Special instructions").
Side effects can be minimized by using the lowest effective dose necessary to control symptoms for the shortest period of time.
For oral use. The recommended daily dose of the drug is 20 - 30 mg per kg of body weight, divided into equal doses, depending on age and body weight, with an interval between doses of 6 - 8 hours. To ensure accurate dosing, the package contains a syringe-doser. The recommended dose should not be exceeded. For short-term use only.
| Age | Body weight (kg) | Recommended dose |
| 3-6 months | 5-7.6 | 2.5 ml of suspension (50 mg) no more than 3 times a day. |
| 6-12 months | 7.7-9 | 2.5 ml of suspension (50 mg) no more than 3-4 times a day. |
| 1-3 years | 10-16 | 5 ml of suspension (100 mg) no more than 3 times a day. |
| 4-6 years | 17-20 | 7.5 ml of suspension (150 mg) no more than 3 times a day. |
| 7-9 years old | 21-30 | 10 ml of suspension (200 mg) no more than 3 times a day. |
| 10-12 years | 31-40 | 15 ml of suspension (300 mg) no more than 3 times a day. |
Do not use on children under 3 months of age unless recommended by a doctor.
Do not use this medicine for children weighing less than 5 kg.
For children aged 3 to 6 months: If symptoms persist for more than 24 hours after the start of treatment or worsen (after 3 doses), you should consult a doctor immediately.
If symptoms persist for more than 3 days after starting treatment or worsen in children aged 6 months to 12 years, a doctor should be consulted.
In case of fever after immunization (children aged 3-6 months), the recommended daily dose is 2.5 ml of suspension (50 mg), if necessary - another 2.5 ml of suspension (50 mg) after 6 hours, but not more than 5 ml of suspension (100 mg) within 24 hours. If symptoms persist, you should consult a doctor.
Patients with sensitive stomachs should take the drug with meals.
Shake before use.
Special categories of patients:
Renal impairment: No dose reduction is required in patients with mild to moderate renal impairment (for patients with severe renal impairment, see section "Contraindications").
Hepatic impairment: No dose reduction is required in patients with mild to moderate hepatic impairment (for patients with severe hepatic impairment, see section "Contraindications").
In case of taking a dose exceeding the recommended dose, you should immediately consult a doctor.
Children
The drug is used in children aged 3 months to 12 years with a body weight of at least 5 kg.
Overdose
In children, symptoms of overdose may occur when taking ibuprofen doses exceeding 400 mg/kg. In adults, dose responses are less pronounced. The half-life in overdose is 1.5-3 hours.
Treatment. There is no specific antidote. Treatment should be symptomatic and supportive, and include maintaining a patent airway and monitoring cardiac function and vital signs until the patient is stable. Consider oral administration of activated charcoal or gastric lavage if the patient has taken a potentially toxic dose within 1 hour. If ibuprofen has already been absorbed, alkaline agents may be used to help eliminate acidic ibuprofen in the urine. Diazepam or lorazepam should be administered intravenously if seizures are frequent or prolonged. Bronchodilators should be administered if asthma is severe. Seek medical attention.
Adverse reactions
The following list of adverse reactions includes all adverse reactions known to occur with ibuprofen, including those observed with high doses, in long-term therapy in patients with rheumatism. The frequency reported, which is beyond the very rare reports, refers to short-term use of doses (maximum 1200 mg ibuprofen per day) for oral dosage forms.
It should be noted that these adverse reactions are mainly dose-dependent and vary individually for each patient.
Adverse reactions that have occurred with ibuprofen are listed below by system organ class and frequency. The frequency of adverse reactions is defined as follows: very common (≥1/10), common (≥1/100 to <1/10), uncommon (≥1/1,000 to <1/100), rare (≥1/10,000 to <1/1,000), very rare (<1/10,000) and not known (cannot be estimated from the available data). Within each frequency grouping, adverse reactions are presented in order of decreasing seriousness.
The most frequently observed adverse reactions are gastrointestinal. In most cases, adverse reactions are dose-dependent, in particular the risk of gastrointestinal bleeding depends on the dose and duration of treatment. Gastrointestinal ulcers, perforation or gastrointestinal bleeding, sometimes fatal, may occur, especially in elderly patients. Nausea, vomiting, diarrhoea, abdominal distension, constipation, dyspepsia, abdominal pain, melena, haematemesis, ulcerative stomatitis, exacerbation of colitis and Crohn's disease have been reported after the use of ibuprofen. Gastritis has been observed less frequently.
Edema, hypertension, and heart failure have been reported to be associated with NSAID treatment.
Clinical trial data and epidemiological data suggest that the use of ibuprofen, especially at high doses of 2400 mg per day and with long-term treatment, may be associated with a slightly increased risk of arterial thrombotic complications (e.g. myocardial infarction or stroke).
There have been reports of exacerbations of inflammation associated with infection, such as necrotizing fasciitis, coinciding with the use of NSAIDs. This may be related to the mechanism of action of NSAIDs.
If signs of infection develop or worsen while taking ibuprofen, the patient is advised to seek immediate medical attention. It is necessary to determine whether antimicrobial/antibiotic therapy is indicated.
With long-term therapy, it is necessary to regularly perform blood tests.
The patient should immediately consult a doctor and stop using ibuprofen if any of the symptoms of hypersensitivity reactions occur, which may develop even with the first use of the drug. In such cases, immediate medical attention is required.
If severe epigastric pain, melena, or bloody vomiting occurs, discontinue use of the drug and consult a doctor immediately.
Infections and invasions.
Very rare: exacerbation of inflammation associated with infection (e.g. development of necrotizing fasciitis. In exceptional cases, chickenpox can cause severe infectious complications of the skin and soft tissues).
From the blood and lymphatic system.
Very rare: blood disorders (anemia, leukopenia, thrombocytopenia, pancytopenia, agranulocytosis). The first signs are fever, sore throat, superficial ulcers in the mouth, flu-like symptoms, severe exhaustion, nasal and skin bleeding, hematomas.
From the immune system.
Hypersensitivity reactions1; uncommon: urticaria and pruritus.
Very rare: severe hypersensitivity reactions, symptoms of which may include swelling of the face, tongue and larynx, shortness of breath, tachycardia, hypotension (anaphylactic reaction, angioedema or severe shock). Exacerbation of asthma.
From the nervous system.
Uncommon: headache, dizziness, insomnia, agitation, irritability or fatigue. Very rare: aseptic meningitis2.
From the side of the cardiac system.
Very rare: heart failure, palpitations, edema, myocardial infarction.
From the vascular system.
Very rare: arterial hypertension, vasculitis.
From the digestive system.
Uncommon: gastric and duodenal ulcers, perforations or gastrointestinal bleeding, melena, haematemesis, sometimes fatal (especially in the elderly), ulcerative stomatitis, gastritis, exacerbation of colitis and Crohn's disease.
Very rare: esophagitis, formation of diaphragmatic strictures of the intestine, pancreatitis.
From the liver.
Very rare: liver dysfunction, liver damage, especially with long-term therapy, liver failure, acute hepatitis.
On the skin and subcutaneous tissue.
Uncommon: various skin rashes1.
Very rare: severe forms of skin reactions such as bullous reactions including Stevens-Johnson syndrome, erythema multiforme and toxic epidermal necrolysis1, alopecia.
Not known: drug reaction with eosinophilia and systemic symptoms (DRESS syndrome); acute generalized exanthematous pustulosis; photosensitivity reactions.
From the respiratory tract and mediastinal organs.
Frequency not known: airway reactivity including asthma, bronchospasm or dyspnoea1.
On the part of the kidneys and urinary system.
Rare: acute renal failure, especially with long-term use of NSAIDs, in combination with increased serum urea. Also includes papillonecrosis.
Very rare: edema, especially in patients with hypertension or renal insufficiency, nephrotic syndrome, interstitial nephritis, which may be accompanied by acute renal failure.
Laboratory studies.
Rare: decreased hemoglobin level.
From the psychological side.
Very rare: psychotic reactions, depression; with prolonged use: hallucinations, confusion.
From the organs of vision.
Frequency unknown: with prolonged treatment, visual disturbances and optic neuritis may occur.
From the hearing organs.
Frequency unknown: dizziness may occur with prolonged treatment.
Rare: ringing in the ears.
General violations.
Frequency unknown: malaise and fatigue.
Description of selected adverse reactions
1 Hypersensitivity reactions have been reported following treatment with ibuprofen. These reactions include (a) non-specific allergic reactions and anaphylaxis, (b) respiratory tract reactions including bronchial asthma, exacerbation of asthma, bronchospasm or dyspnoea, or (c) various skin disorders including rashes of various types, pruritus, urticaria, purpura, angioedema and, more rarely, exfoliative and bullous dermatoses (including epidermal necrolysis, Stevens-Johnson syndrome and erythema multiforme).
2 The mechanism of pathogenesis of drug-induced aseptic meningitis is not fully understood. However, available data on aseptic meningitis associated with NSAIDs suggest a hypersensitivity reaction (due to temporal relationship to drug intake and resolution of symptoms after drug withdrawal). In particular, isolated cases of symptoms of aseptic meningitis (such as neck stiffness, headache, nausea, vomiting, fever or disorientation) have been observed during treatment with ibuprofen in patients with pre-existing autoimmune disorders (such as systemic lupus erythematosus, mixed connective tissue disease).
Expiration date
3 years.
Storage conditions
Store out of the reach of children at a temperature not exceeding 25 °C.
Packaging
100 ml or 200 ml of suspension in a bottle. Bottle in a cardboard box complete with a dosing syringe.
Vacation category
Without a prescription.
Producer
Reckitt Benckiser Healthcare (UK) Limited.
Location of the manufacturer and its business address
Densom Lane, Hull, HU8 7DS, United Kingdom.
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.