Onivide pegylated liposomal concentrate for infusion 4.3 mg/ml vial 10 ml No. 1
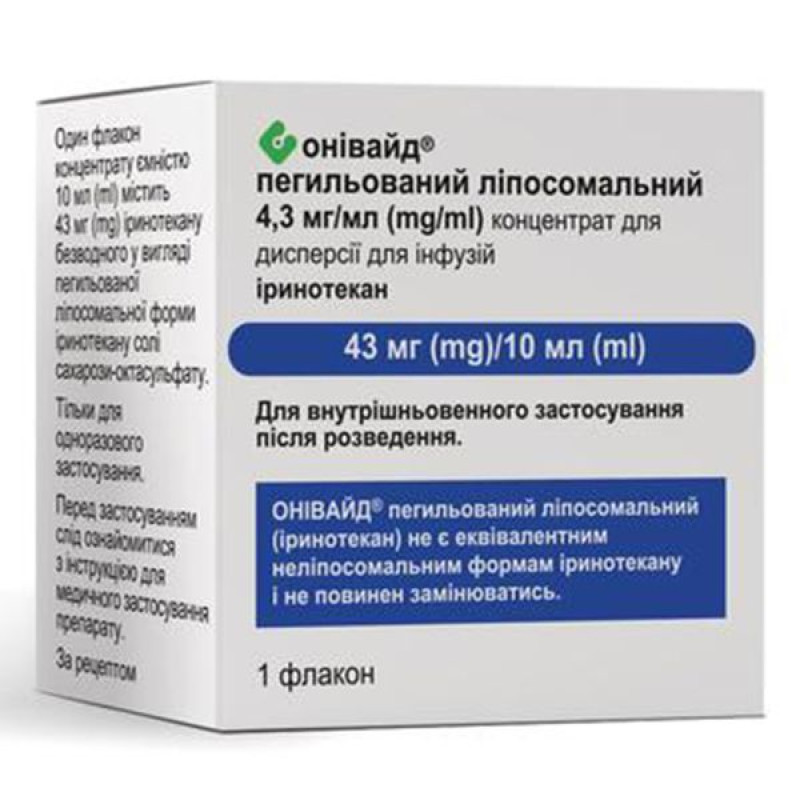
Instructions Onivide pegylated liposomal concentrate for infusion 4.3 mg/ml vial 10 ml No. 1
Composition
active ingredients: irinotecan;
One 10 ml vial of concentrate contains 43 mg of irinotecan anhydrous (as pegylated liposomal irinotecan sucrose octasulfate salt).
1 ml of concentrate contains 4.3 mg of irinotecan anhydrous (as pegylated liposomal form of irinotecan sucrose octasulfate salt);
excipients: sucrose octasulfate, 1,2-distearoyl-sn-glycero-3-phosphocholine (DSPC), cholesterol, M-(carbonyl-methoxypolyethylene glycol-2000)-1,2-distearoyl-sn-glycero-3-phosphoethanolamine (MPEG-2000-DSPE), 2-[4-(2-hydroxyethyl)piperazin-1-yl]ethanesulfonic acid (HEPES buffer), sodium chloride, water for injections.
Dosage form
Concentrate for dispersion for infusions.
Main physicochemical properties: opaque isotonic liposomal dispersion from white to slightly yellow. The concentrate has a pH of 7.2 and an osmolarity of 295 mosmol/kg.
Pharmacotherapeutic group
Topoisomerase 1 (TOP1) inhibitors. ATX code: L01CE02.
Pharmacological properties
Pharmacodynamics.
Mechanism of action. The active substance of ONIVYDE® pegylated liposomal is irinotecan (a topoisomerase I inhibitor) encapsulated in a lipid bilayer vesicle or liposome.
Irinotecan is a derivative of camptothecin. Camptothecin acts as a specific inhibitor of the enzyme DNA topoisomerase I. Irinotecan and its active metabolite SN 38 reversibly bind to the DNA topoisomerase I complex and induce single-strand DNA damage, which blocks the DNA replication fork and causes cytotoxicity. Irinotecan is metabolized by carboxylesterase to the compound SN 38. SN 38 is approximately 1,000 times more potent than irinotecan as an inhibitor of topoisomerase I isolated from human and rodent tumor cell lines.
Pharmacodynamic effects: In experimental animal models, ONIVYDE® pegylated liposomal showed sustained plasma concentrations of irinotecan and SN 38 at the tumor site.
Clinical efficacy and safety. The safety and efficacy of ONIVYDE® pegylated liposomal were studied in an international randomized, open-label, controlled clinical trial (NAPOLI-1) that investigated two treatment regimens in patients with metastatic pancreatic adenocarcinoma with documented disease progression after gemcitabine or gemcitabine-based therapy. The study was conducted to evaluate the clinical efficacy and safety of ONIVYDE® pegylated liposomal monotherapy or the combination of ONIVYDE® pegylated liposomal + 5-FU/LV compared to an active control group receiving 5-FU/LV. The primary inclusion criteria for patients with metastatic pancreatic adenocarcinoma in the NAPOLI-1 study were a Karnowski Performance Status Score (KPS) ≥ 70, normal bilirubin, transaminases ≤ 2.5 times the upper limit of normal (ULN) or ≤ 5 times the ULN for patients with liver metastases, and albumin ≥ 3.0 g/dL. A total of 417 patients were randomized to ONIVYDE® pegylated liposomal + 5-FU/LV (n = 117), ONIVYDE® pegylated liposomal monotherapy (n = 151), and 5-FU/LV (n = 149). Patient demographics and baseline disease characteristics were balanced between study arms. Patients were treated until disease progression or unacceptable toxicity. The primary efficacy endpoint was overall survival (OS). Additional efficacy endpoints included progression-free survival (PFS) and objective response rate (ORR). Results are presented in Table 1.
Table 1: Results of the NAPOLI-1 clinical trial
liposomal + 5-FU/LV ( (n = 117) | 5-FU/LV (n = 119) | |
| Overall survival1 | ||
| Number of fatalities, n (%) | 75 (64) | 80 (67) |
| Median OS (months) | 6.1 | 4.2 |
| (95% CI) | (4.8; 8.9) | (3.3; 5.3) |
Relative risk (95% CI)3 | 0.67 (0.49–0.92) | |
| p-value4 | 0.0122 | |
| Progression-free survival1,2 | ||
| Death or progression, n (%) | 83 (71) | 92 (77) |
| Median PFS (months) | 3.1 | 1.5 |
| (95% CI) | (2.7; 4.2) | (1.4; 1.8) |
| Relative risk (95% CI)3 | 0.56 (0.41–0.75) | |
| p-value4 | 0.0001 | |
| Objective response rate2 | ||
| n | 19 | 1 |
| CHW (%) | 16.2 | 0.8 |
| 95% CI of frequency5 | 9.6; 22.9 | 0.0; 2.5 |
| Frequency difference (95% CI)5 | 15.4 (8.5; 22.3) | |
| p-value6 | < 0.0001 |
1 Median - an estimate of the average survival time according to the Kaplan-Meier method.
2 According to the Response Evaluation Criteria in Solid Tumors (RECIST) guidelines, revision 1.1.
3 Cox model analysis.
4 Unstratified log-rank test.
5 Based on normal approximation.
6 Fisher's exact test.
In a small number of patients who had previously received non-liposomal forms of irinotecan, no benefit of ONIVYDE® pegylated liposomal was demonstrated.
Pharmacokinetics.
Absorption. Liposomal encapsulation of irinotecan prolongs its circulation and limits its distribution compared to non-liposomal forms of irinotecan. The plasma pharmacokinetics of total irinotecan and total SN-38 were evaluated in cancer patients receiving ONIVYDE® pegylated liposomal as monotherapy or as part of combination chemotherapy at doses ranging from 50 to 155 mg/m2. The pharmacokinetic parameters of total irinotecan and SN-38 after administration of ONIVYDE® pegylated liposomal at a dose of 70 mg/m2 are presented in Table 2.
Table 2. Summary of Mean Values (± Standard Deviation) of Total Irinotecan and Total SN-38
| Indicator | FC parameters | Unit of measurement | Geometric mean ONIVYDE® pegylated liposomal (95% CI)a 70 mg/m2 (n=353)b | Mean non-liposomal irinotecan (SV) 125 mg/m2 (n=99)s |
| Generic Irinotecan | AUC | h×ng/ml | 919 228 (845 653-999 204) | 10,529 (3,786) |
| Сmax | ng/ml | 28,353 (27,761-28,958) | 1,492 (452) | |
| Ground clearance (CL) | l/h/m2 | 0.087 (0.080-0.094) | 13.0 (5,6) | |
| Volume (V) | l/m2 | 2.6 (2.6-2.7) | 138 (60.9) | |
| t1/2 effective | hour | 20.8 (19.4-22.3) | 6.07 (1.19) | |
| Indicator | FC parameters | Unit of measurement | Geometric mean ONIVYDE® pegylated liposomal (95% CI)a 70 mg/m2 (n=353)b | Mean non-liposomal irinotecan (SV) 125 mg/m2 (n=99)s |
| General SN-38 | AUC | h×ng/ml | 341 (326-358) | 267 (115) |
| Сmax | ng/ml | 3.0 (2.9-3.1) | 27.8 (11.6) | |
| t1/2 effective | hour | 40.9 (39.8-42.0) | 11.7 (4.29) |
SD = standard deviation.
AUC = area under the plasma concentration curve (extrapolated to infinity for ONIVYDE® pegylated liposomal and AUC24h for non-liposomal irinotecan).
Cmax = maximum plasma concentration.
t1/2 effective = effective half-life.
a Values calculated from population PK analysis.
b n = 353 refers to all subjects included in the population PK analysis.
c Values are derived from published data [Schaaf LJ et al. Clin Cancer Res. 2006 Jun 15; 12:3782-91].
Distribution: Direct measurement of liposomal irinotecan shows that 95% of irinotecan remains encapsulated in liposomes during circulation. The non-liposomal form of irinotecan exhibits a large volume of distribution (138 l/m2). The volume of distribution of ONIVYDE® pegylated liposomal at a dose of 70 mg/m2 was 2.6 l/m2, indicating that ONIVYDE® pegylated liposomal is primarily confined to the vascular fluid. The binding of ONIVYDE® pegylated liposomal to plasma proteins is negligible (< 0.44% of total irinotecan in the formulation). The binding of non-liposomal irinotecan to plasma proteins is moderate (30% to 68%), while SN-38 has a high degree of binding to human plasma proteins (approximately 95%).
Biotransformation. Irinotecan released from liposomal encapsulation undergoes a metabolic pathway similar to that described for the non-liposomal form of irinotecan. Metabolic transformation of irinotecan to the active metabolite SN-38 is mediated by the enzyme carboxylesterase. In vitro studies have shown that irinotecan, SN-38 and another metabolite, aminopentanecarboxylic acid (APA), do not inhibit cytochrome P-450 isoenzymes. SN-38 is subsequently conjugated primarily by the enzyme UDP-glucuronosyltransferase 1A1 (UGT1A1) to form a glucuronide metabolite. UGT1A1 activity is reduced in individuals with genetic polymorphisms that result in reduced enzyme activity, such as the UGT1A1*28 polymorphism. Based on a population pharmacokinetic analysis in patients receiving ONIVYDE® pegylated liposomal (for the subgroup with UGT1A1*28 genotypic testing, the analysis was adapted for the lower dose administered to patients homozygous for the UGT1A1*28 allele), the mean steady-state concentration of total SN-38 was 1.06 and 0.95 ng/mL in patients homozygous (n=14) and non-homozygous (n=244) for this allele, respectively.
Excretion. The excretion of ONIVYDE® pegylated liposomal and non-liposomal irinotecan in humans has not been fully studied. Urinary excretion of non-liposomal irinotecan is 11% - 20%; SN-38 < 1%, and SN-38 glucuronide - 3%. Total biliary and renal excretion of irinotecan and its metabolites (SN-38 and SN-38 glucuronide) within 48 hours after administration of non-liposomal irinotecan in two patients ranged from approximately 25% (100 mg/m2) to 50% (300 mg/m2).
Hepatic impairment: No specific pharmacokinetic studies have been conducted in patients with hepatic impairment. In a population pharmacokinetic analysis, patients with baseline total bilirubin levels of 1-2 mg/dL (n=19) demonstrated a 37% increase in mean steady-state total SN-38 concentrations (0.98 [95% CI: 0.94-1.02] and 1.29 [95% CI: 1.11-1.5] ng/mL, respectively) compared to those with baseline bilirubin levels < 1 mg/dL (n=329); however, there was no effect of elevated ALT/AST on total SN-38 concentrations. Data are not available for patients with total bilirubin levels greater than twice the ULN.
Other special categories of patients.
Age and gender: A population pharmacokinetic analysis in patients aged 28 to 87 years, 11% of whom were ≥75 years, suggests that age has no clinically significant effect on irinotecan and SN-38 concentrations.
A population pharmacokinetic analysis in 196 male and 157 female patients suggests that gender has no clinically significant effect on irinotecan and SN-38 concentrations after adjustment for BSA.
Race: Population pharmacokinetic analysis suggests that Asian patients have 56% lower mean steady-state concentrations of total irinotecan (3.93 [95% CI: 3.68-4.2] and 1.7-4 [95% CI: 1.58-1.93] mg/L, respectively) and 8% higher mean steady-state concentrations of total SN-38 (0.97 [95% CI: 0.92-1.03] and 1.05 [95% CI: 0.98-1.11] ng/mL, respectively) than Caucasian patients.
Relationship between pharmacokinetics and pharmacodynamics. In a pooled analysis of 353 patients, higher plasma Cmax of SN-38 was associated with an increased likelihood of neutropenia, and higher Cmax of total irinotecan was associated with diarrhea.
In a clinical trial of ONIVYDE® pegylated liposomal efficacy, higher plasma concentrations of total irinotecan and SN-38 in patients treated with ONIVYDE® pegylated liposomal + 5-FU/LV were associated with longer OS and PFS, as well as a higher PFS.
Indication
Treatment of metastatic pancreatic adenocarcinoma in combination with 5-fluorouracil (5-FU) and leucovorin (LV) in adult patients with disease progression following gemcitabine-based therapy.
Contraindication
History of severe hypersensitivity to irinotecan or to any of the excipients.
Breastfeeding (see section "Use during pregnancy or breastfeeding").
Special safety precautions
ONIVYDE® pegylated liposomal is a cytotoxic medicinal product and caution should be exercised when handling it. Protective gloves, safety glasses and protective clothing are recommended when handling or administering ONIVYDE® pegylated liposomal. If the dispersion comes into contact with the skin, the skin should be washed immediately and thoroughly with soap and water. If the dispersion comes into contact with mucous membranes, they should be washed thoroughly with water. Given the cytotoxic nature of ONIVYDE® pegylated liposomal, pregnant healthcare professionals should avoid contact with it.
Interaction with other medicinal products and other types of interactions
Information on drug interactions with ONIVYDE® pegylated liposomal is based on data from the scientific literature on non-liposomal forms of irinotecan.
Interactions affecting the use of ONIVIDE® pegylated liposomal
Strong CYP3A4 inducers. In patients receiving non-liposomal irinotecan and anticonvulsants that induce CYP3A4 (phenytoin, phenobarbital or carbamazepine), significant decreases in irinotecan concentrations (12% decrease in AUC with St. John's wort, 57%-79% with phenytoin, phenobarbital or carbamazepine) and SN-38 (42% decrease in AUC with St. John's wort, 36%-92% with phenytoin, phenobarbital or carbamazepine) have been observed. Therefore, concomitant use of ONIVYDE pegylated liposomal with CYP3A4 inducers may result in decreased systemic exposure.
CYP3A4 inhibitors and potent UGT1A1 inhibitors. In patients receiving non-liposomal irinotecan and ketoconazole, both CYP3A4 and UGT1A1 inhibitors, an increase in SN-38 concentrations by 109% was observed. Therefore, concomitant use of ONIVYDE® pegylated liposomal with other CYP3A4 inhibitors (e.g. grapefruit juice, clarithromycin, indinavir, itraconazole, lopinavir, ezetimibe, nelfinavir, ritonavir, saquinavir, telaprevir, voriconazole) may increase its systemic concentration. Given the drug interaction of non-liposomal irinotecan and ketoconazole, concomitant use of ONIVYDE® pegylated liposomal with other UGT1A1 inhibitors (e.g. azathioprine, gemfibrozil, indinavir) may also increase its systemic concentration.
Based on the results of a population pharmacokinetic analysis, the simultaneous use of ONIVYDE® pegylated liposomal + 5-FU/LV does not change the pharmacokinetics of ONIVYDE® pegylated liposomal.
Antineoplastic agents (including flucytosine as a 5-FU derivative): Adverse reactions of irinotecan, such as myelosuppression, may be potentiated by other antineoplastic agents with a similar adverse reaction profile.
Interactions of ONIVIDE® pegylated liposomal with other drugs have not been established.
Application features
General. ONIVYDE® pegylated liposomal is a liposomal formulation of irinotecan with different pharmacokinetic properties compared to non-liposomal irinotecan. The dose concentration and potency are different compared to non-liposomal irinotecan formulations.
ONIVYDE® pegylated liposomal is not equivalent to other non-liposomal formulations of irinotecan and should not be substituted. In a limited number of patients previously treated with non-liposomal formulations of irinotecan, no benefit of ONIVYDE® pegylated liposomal has been demonstrated.
Myelosuppression/neutropenia. Monitoring of complete blood counts is recommended during treatment with ONIVYDE® pegylated liposomal. Patients should be advised of the risk of neutropenia and the severity of fever. The median time to maximum neutrophil decline ≥ grade 3 neutropenia was 23 days (range 8 to 104) after the first dose of ONIVYDE® pegylated liposomal. Febrile neutropenia (body temperature >38°C and neutrophil count ≤1,000 cells/mm3) should be treated promptly in a hospital setting with broad-spectrum intravenous antibiotics. ONIVYDE® pegylated liposomal should be withheld if neutropenic fever occurs or if the absolute neutrophil count falls to <1,500 cells/mm3. Cases of sepsis with neutropenic fever and subsequent septic shock, with fatal outcome, have been reported in patients with metastatic pancreatic adenocarcinoma treated with ONIVYDE® pegylated liposomal. In patients who experience severe hematological events, dose reduction or discontinuation is recommended (see section 4.2). ONIVYDE® pegylated liposomal should not be used in patients with severe bone marrow failure.
A history of intra-abdominal irradiation increases the risk of severe and febrile neutropenia with ONIVYDE® pegylated liposomal. Close monitoring of blood cell counts and consideration of myeloid growth factors are recommended in patients with a history of intra-abdominal irradiation. Caution should be exercised in patients undergoing irradiation while receiving ONIVYDE® pegylated liposomal.
Patients with impaired bilirubin glucuronidation, such as Gilbert's syndrome, may be at higher risk of myelosuppression when receiving ONIVYDE® pegylated liposomal.
Asian patients, compared with Caucasian patients, are at increased risk of severe and febrile neutropenia after treatment with ONIVYDE® pegylated liposomal + 5-FU/LV (see sections “Adverse reactions” and “Pharmacokinetics”).
Immunosuppressive effect and vaccines. The use of live or live attenuated vaccines in patients immunocompromised by chemotherapeutic agents, including ONIVIDE® pegylated liposomal, may result in serious or fatal infections; therefore, vaccination with live vaccines should be avoided. Killed or inactivated vaccines may be used, but the response to such agents may be diminished.
Interaction with strong CYP3A4 inducers. ONIVYDE® pegylated liposomal should not be used concomitantly with strong CYP3A4 inducers such as anticonvulsants (phenytoin, phenobarbital or carbamazepine), rifampin, rifabutin and St. John's wort, unless no therapeutic alternatives are available. An appropriate starting dose for patients taking such anticonvulsants or other strong inducers has not been established. Consideration should be given to switching these medicinal products to non-enzyme inducers at least two weeks prior to initiating ONIVYDE® pegylated liposomal therapy (see section 4.5).
Interaction with strong CYP3A4 inhibitors or strong UGTIA1 inhibitors. ONIVYDE® pegylated liposomal should not be used concomitantly with strong CYP3A4 inhibitors (e.g. grapefruit juice, clarithromycin, indinavir, itraconazole, lopinavir, nefazodone, nelfinavir, ritonavir, saquinavir, telaprevir, voriconazole). Use of strong CYP3A4 inhibitors should be discontinued at least one week prior to initiating therapy with ONIVYDE® pegylated liposomal.
Diarrhea: Early (≤ 24 hours after initiation of administration) or delayed (> 24 hours) diarrhea may occur with ONIVYDE® pegylated liposomal (see Adverse Reactions). If early diarrhea occurs, therapeutic and prophylactic use of atropine should be considered unless contraindicated. Patients should be warned of the risk of delayed diarrhea, which can be debilitating and, in rare cases, life-threatening, as persistent loose or watery stools may lead to dehydration, electrolyte imbalance, colitis, gastrointestinal (GI) ulceration, infection, or sepsis.
As soon as the first loose stools occur, the patient should start drinking plenty of fluids containing electrolytes. Patients should have loperamide (or a similar product) available to start treatment for delayed diarrhoea. Loperamide should be started at the first appearance of loose or loose stools or more frequent than usual stools. Loperamide should be used until the patient has been free of diarrhoea for at least 12 hours. If diarrhoea persists for more than 24 hours with loperamide, additional oral antibiotics (e.g. fluoroquinolone for 7 days) should be considered. Loperamide should not be used for more than 48 hours in a row because of the risk of paralytic ileus. If diarrhoea persists for more than 48 hours, loperamide should be discontinued, electrolytes should be monitored and maintained with fluids, and the antibiotic should be continued until associated symptoms resolve.
Treatment with ONIVYDE® pegylated liposomal should be delayed until diarrhea has resolved to ≤ Grade 1 (2-3 more bowel movements per day than before treatment). ONIVYDE® pegylated liposomal is not recommended for use in patients with ileus and chronic inflammatory bowel disease until they have resolved. If Grade 3 or 4 diarrhea occurs, the next dose of ONIVYDE® pegylated liposomal should be reduced (see Dosage and Administration).
Cholinergic reactions: Early diarrhea may be accompanied by cholinergic symptoms such as rhinitis, hypersalivation, flushing, increased sweating, bradycardia, miosis, and hyperperistalsis. Atropine should be used if cholinergic symptoms occur.
Acute infusion and related reactions. Infusion reactions, mainly rash, urticaria, periorbital edema, or pruritus, have been reported in patients receiving ONIVYDE® pegylated liposomal. The first-time events (all Grade 1 or 2) occurred primarily at the start of ONIVYDE® pegylated liposomal treatment, with only 2 out of 10 patients reporting such events after the fifth dose. Hypersensitivity reactions, including acute infusion reaction, anaphylactic/anaphylactoid reactions, and angioedema, may occur. In the event of severe hypersensitivity reactions, ONIVYDE® pegylated liposomal should be discontinued.
Previous Whipple procedure: Patients with a history of Whipple procedure are at increased risk of developing serious infections after the use of ONIVYDE® pegylated liposomal in combination with 5-FU and a drug (see section 4.8). Patients should be monitored for signs of infection.
Vascular disorders. The use of ONIVYDE® pegylated liposomal has been associated with thromboembolic events such as pulmonary embolism, venous thrombosis, and arterial thromboembolism. A careful medical history should be taken to identify individuals with multiple risk factors in addition to the underlying tumor. Patients should be warned about the signs and symptoms of thromboembolism and advised to contact their doctor or nurse immediately if such signs or symptoms occur.
Hepatic impairment. Higher concentrations of total SN-38 have been observed in patients with hyperbilirubinemia (see section "Pharmacokinetics") and, therefore, an increased risk of neutropenia. Patients with total bilirubin 1.0-2.0 mg/dL should have regular monitoring of complete blood count results. Caution should be exercised in patients with hepatic impairment (bilirubin > 2 times ULN; transaminases > 5 times ULN). ONIVYDE® pegylated liposomal in combination with other hepatotoxic drugs, especially in the presence of hepatic impairment, should be used with caution.
Renal impairment: ONIVYDE® pegylated liposomal has not been studied in patients with severe renal impairment (see Pharmacokinetics).
Underweight patients (body mass index < 18.5 kg/m2). In a clinical trial evaluating ONIVYDE® pegylated liposomal + 5-FU/LV, 5 of 8 underweight patients experienced grade 3 or 4 adverse reactions, mainly myelosuppression, while 7 of 8 cases required dose modifications such as dose delays, dose reductions, or drug discontinuation. ONIVYDE® pegylated liposomal should be used with caution in patients with a body mass index < 18.5 kg/m2.
Excipients: One vial of this medicinal product contains 33.1 mg of sodium, equivalent to 1.65% of the WHO recommended maximum daily intake of 2 g sodium for adults.
Use during pregnancy or breastfeeding
Women of childbearing potential/contraception for women and men. Women of childbearing potential should use effective methods of contraception during treatment with ONIVYDE® pegylated liposomal and for 7 months after treatment. Men should use condoms during treatment with ONIVYDE® pegylated liposomal and for 4 months after treatment.
Pregnancy. There are no adequate data from the use of ONIVYDE® pegylated liposomal in pregnant women. In animal studies, irinotecan has been shown to be embryotoxic and teratogenic, and it is therefore likely that ONIVYDE® pegylated liposomal may cause fetal harm when administered during pregnancy. Therefore, based on the animal studies and the mechanism of action of irinotecan, ONIVYDE® pegylated liposomal should not be used during pregnancy unless clearly necessary. If ONIVYDE® pegylated liposomal is used during pregnancy or if the patient becomes pregnant while receiving therapy, the patient should be apprised of the potential hazard to the fetus.
Breastfeeding. It is not known whether ONIVYDE® pegylated liposomal or its metabolites are excreted in human milk. Because of the potential for serious adverse reactions in breastfed infants, treatment with ONIVYDE® pegylated liposomal is contraindicated during breast-feeding (see Contraindications). Patients should not breast-feed for one month after the last dose.
Fertility. There are no data on the effect of ONIVYDE® pegylated liposomal on human fertility. Animal studies have shown that non-liposomal formulations of irinotecan caused atrophy of male and female reproductive organs after multiple daily doses of irinotecan. Before starting ONIVYDE® pegylated liposomal, it is advisable to advise the patient on gamete preservation.
Ability to influence reaction speed when driving vehicles or other mechanisms
ONIVYDE® pegylated liposomal has a moderate effect on the speed of reaction when driving or using other mechanisms. During treatment, patients should exercise caution when driving or using other mechanisms.
Method of administration and doses
The prescription and administration of ONIVIDE® pegylated liposomal to patients should be carried out exclusively by medical specialists who have experience in anticancer therapy.
ONIVYDE® pegylated liposomal is not equivalent to non-liposomal forms of irinotecan and should not be substituted.
Dosage
ONIVYDE® pegylated liposomal, leucovorin and 5-fluorouracil are administered sequentially. The recommended dose and schedule of ONIVYDE® pegylated liposomal is 70 mg/m2 intravenously over 90 minutes followed by leucovorin at a dose of 400 mg/m2 intravenously over 30 minutes and 5-FU at 2,400 mg/m2 intravenously over 46 hours every 2 weeks. ONIVYDE® pegylated liposomal is not used as monotherapy.
Premedication: At least 30 minutes prior to the start of ONIVYDE® pegylated liposomal infusion, patients are recommended to be premedicated with standard doses of dexamethasone (or equivalent corticosteroid) together with a 5-HT3 antagonist (or other antiemetic).
Dose adjustment. All dose adjustments should be based on the previous highest grade of toxicity. No dose adjustment is required for leucovorin. No dose adjustment is recommended for Grades 1 and 2 toxicity. Dose adjustment recommendations for Grades 3 and 4 toxicity associated with ONIVYDE® pegylated liposomal are provided in Tables 3 and 4. For patients who initiate treatment with ONIVYDE® pegylated liposomal at 50 mg/m2 and do not increase to 70 mg/m2, a first dose reduction to 43 mg/m2 and a second dose reduction to 35 mg/m2 are recommended. Patients who require a further dose reduction are advised to discontinue treatment. Patients homozygous for the UGT1A1*28 allele who do not experience toxicity related to ONIVYDE® pegylated liposomal during the first cycle of therapy (reduced dose - 50 mg/m2) may have their dose increased to a total of 70 mg/m2 in subsequent cycles depending on individual tolerability.
Table 3. Recommendations for dose adjustment of ONIVYDE® pegylated liposomal + 5-FU/LV for grade 3-4 toxicity in patients not homozygous for the UGT1A1*28 allele
| Toxicity grade (value) according to NCI STCAE Rev. 4.01 | Dose adjustment of ONIVYDE® pegylated drugs liposomal/5-FU (for patients not homozygous for the UGT1A1*28 allele) | |
| Hematological symptoms of toxicity | ||
| Neutropenia | Do not start a new cycle of therapy until an absolute neutrophil count ≥ 1,500 cells/mm3 is achieved | |
| Grade 3 or 4 (< 1,000 cells/mm3) or febrile neutropenia | First case | Reduce ONIVYDE® pegylated liposomal dose to 50 mg/m2 Reduce 5-FU dose by 25% (1,800 mg/m2) |
| Second case | Reduce ONIVYDE® pegylated liposomal dose to 43 mg/m2 Reduce the dose of 5-FU by an additional 25% (1,350 mg/m2). | |
| Third case | Stop treatment | |
Thrombocytopenia Leukopenia | Do not start a new cycle of therapy until platelet count ≥ 100,000/mm3 is achieved Dose adjustments for leukopenia and thrombocytopenia are based on the NCI CTCAE toxicity classification and are similar to those recommended above for neutropenia. | |
| Non-hematological symptoms of toxicity2 | ||
| Diarrhea | Do not start a new cycle of therapy until diarrhea severity has decreased to ≤ Grade 1 (2-3 more bowel movements per day than before treatment) | |
| Level 2 | Do not start a new cycle of therapy until diarrhea severity has decreased to ≤ Grade 1 (2-3 more bowel movements per day than before treatment) | |
| Grade 3 or 4 | First case | Reduce ONIVYDE® pegylated liposomal dose to 50 mg/m2 Reduce 5-FU dose by 25% (1,800 mg/m2) |
| Second case | Reduce ONIVYDE® pegylated liposomal dose to 43 mg/m2 Reduce 5-FU dose by an additional 25% (1,350 mg/m2) | |
| Third case | Stop treatment | |
| Nausea/vomiting | Do not start a new cycle of therapy until nausea/vomiting has resolved to ≤ Grade 1 or to baseline | |
Grade 3 or 4 (despite antiemetic therapy) | First case | Optimize antiemetic therapy Reduce the dose of ONIVYDE® pegylated liposomal to 50 mg/m2 |
| Second case | Optimize antiemetic therapy Reduce ONIVYDE® pegylated liposomal dose to 43 mg/m2 | |
| Third case | Stop treatment |
| Toxic manifestations from the side
Specifications
Characteristics
Active ingredient
Irinotecan
Adults
Can
Country of manufacture
France
Diabetics
Can
Dosage
4.3 mg/ml
Drivers
With caution
For allergies
With caution
For children
It is impossible.
Form
Infusions
Method of application
Injections
Nursing
It is impossible.
Pregnant
In case of emergency, as prescribed by a doctor
Producer
Servier Laboratories
Quantity per package
1 bottle
Trade name
Oniwide
Vacation conditions
By prescription
Reviews
There are no reviews for this product. There are no reviews for this product, be the first to leave your review.
Answers & questions
Add your question and we will answer as soon as possible.
No questions about this product, be the first and ask your question.
You are watched
Zarsio solution for injection and infusion 48 million IU 0.5 ml in pre-filled syringe No. 5
In stock
7 105.53 грн.
|










