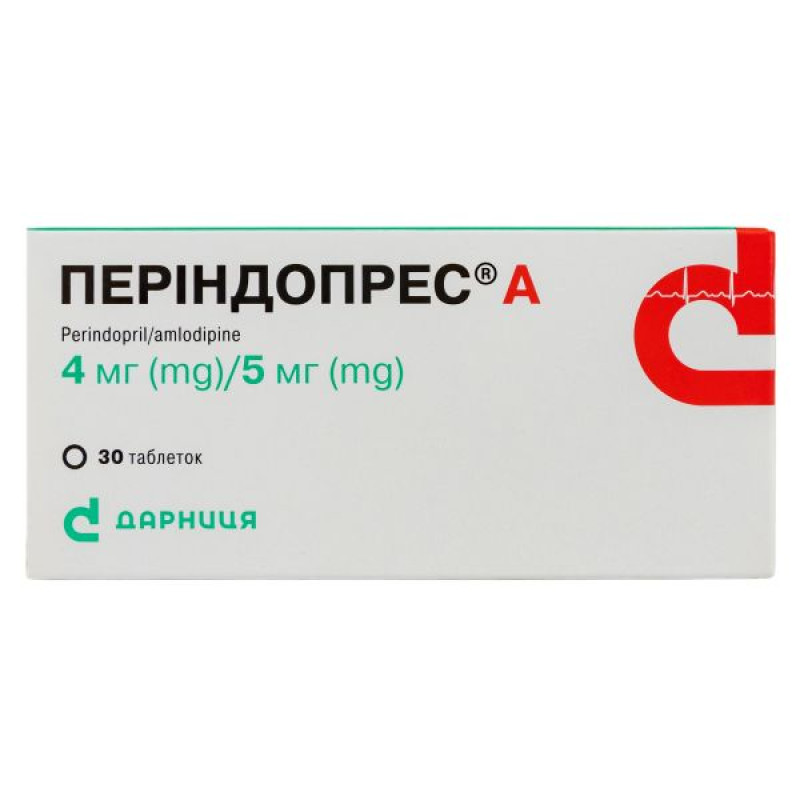
Perindopres A tablets 4 mg + 5 mg No. 30

Instructions for Perindopress A tablets 4 mg + 5 mg No. 30
Composition
active ingredients: perindopril/amlodipine
PERINDOPRES® A 4 mg/5 mg
1 tablet contains: perindopril tert-butylamine 4 mg (equivalent to 3.338 mg perindopril) and amlodipine besylate 6.935 mg (equivalent to 5 mg amlodipine);
Excipients: lactose monohydrate, microcrystalline cellulose, colloidal hydrophobic silicon dioxide, magnesium stearate.
PERINDOPRES® A 8 mg/10 mg
1 tablet contains: perindopril tert-butylamine 8 mg (equivalent to 6.676 mg perindopril) and amlodipine besylate 13.870 mg (equivalent to 10 mg amlodipine);
Excipients: lactose monohydrate, microcrystalline cellulose, colloidal hydrophobic silicon dioxide, magnesium stearate.
Dosage form
Pills.
Main physicochemical properties:
PERINDOPRES® A 4 mg/5 mg: white or almost white, flat-cylindrical tablets with a bevel.
PERINDOPRES® A 8 mg/10 mg: white or almost white, flat-cylindrical tablets with a bevel.
Pharmacotherapeutic group
ACE inhibitors, combinations. ACE inhibitors and calcium channel blockers. Perindopril and amlodipine. ATC code C09B B04.
Pharmacological properties
Pharmacodynamics.
Perindopril
Perindopril is an inhibitor of the enzyme that converts angiotensin I to angiotensin II, angiotensin-converting enzyme (ACE). The converting enzyme or kinase is an exopeptidase that enables the conversion of angiotensin I to the vasoconstrictor angiotensin II and also causes the breakdown of the vasodilator bradykinin to an inactive heptapeptide. Inhibition of ACE leads to a decrease in the concentration of angiotensin II in the blood plasma, which increases the activity of plasma renin (by inhibiting the negative feedback on renin release) and reduces the secretion of aldosterone. Since ACE inactivates bradykinin, inhibition of ACE also leads to an increase in the activity of the circulating and local kallikrein-kinin system (and thus also leads to the activation of the prostaglandin system). This mechanism of action is responsible for the blood pressure lowering effect of ACE inhibitors and is partly responsible for some of their side effects (e.g., cough).
Perindopril acts through its active metabolite, perindoprilat. Other metabolites do not demonstrate activity in inhibiting ACE under experimental conditions.
Clinical efficacy and safety
Arterial hypertension
Perindopril effectively lowers blood pressure in all degrees of arterial hypertension - mild, moderate and severe. The reduction in systolic and diastolic blood pressure is observed both in the supine and standing positions.
Perindopril reduces peripheral vascular resistance, which leads to a decrease in blood pressure. As a result, peripheral blood flow increases without affecting heart rate. Renal blood flow usually increases, while glomerular filtration rate does not change. The maximum antihypertensive effect develops 4-6 hours after a single dose and persists for at least 24 hours: the T/P ratio (maximum efficacy/minimum efficacy during the day) of perindopril is 87-100%. Blood pressure decreases rapidly. In patients who respond to treatment, normalization of blood pressure occurs within a month and is maintained without the occurrence of tachyphylaxis. If perindopril is discontinued, there is no withdrawal effect. Perindopril reduces left ventricular hypertrophy. Clinical studies have shown that perindopril has vasodilatory properties. It improves the elasticity of large arteries and reduces the ratio of wall thickness to lumen in small arteries.
Prevention of cardiovascular complications in patients with proven stable coronary heart disease (CHD)
The EUROPA study is an international multicenter, randomized, double-blind, placebo-controlled clinical trial that lasted 4 years. 12,218 adult patients were randomized into groups: 6,110 patients received 8 mg of perindopril tert-butylamine (equivalent to 10 mg perindopril arginine) and 6,108 patients received placebo. The study included patients with confirmed coronary artery disease and without clinically confirmed heart failure. Overall, 90% of patients had a history of myocardial infarction and/or revascularization surgery. Most patients in the study received perindopril in addition to standard therapy: antiplatelet agents, lipid-lowering drugs and β-blockers. The main efficacy endpoint was a composite of cardiovascular mortality, non-fatal myocardial infarction and/or cardiac arrest with subsequent successful resuscitation. The result of therapy with perindopril tertbutylamine at a dose of 8 mg (equivalent to perindopril arginine 10 mg) once daily was a significant absolute reduction in the primary endpoint of the study by 1.9% (relative risk reduction by 20%, 95% CI [9.4; 28.6] – p<0.001).
Amlodipine
The mechanism of antihypertensive action of amlodipine is due to a direct relaxant effect on vascular smooth muscle. The exact mechanism by which amlodipine reduces angina is not fully understood, but amlodipine reduces overall exercise ischemia through the following actions:
amlodipine dilates peripheral arterioles and thus reduces total peripheral resistance (afterload). Since the heart rate does not change, the reduction in workload on the heart reduces myocardial energy consumption and oxygen demand;
Amlodipine also partially dilates the main coronary arteries and coronary arterioles in both intact and ischemic areas of the myocardium. This dilation increases oxygen delivery to the myocardium in patients with vasospastic angina (Prinzmetal's angina or variant angina).
In patients with hypertension, once-daily administration of amlodipine provides clinically significant reductions in supine and standing blood pressure over 24 hours. Due to its slow onset of action, amlodipine does not cause acute hypotension.
In patients with angina pectoris, once-daily administration of amlodipine increases total exercise time, time to angina attack, and time to 1 mm ST-segment depression, reduces the frequency of angina attacks, and reduces the need for nitroglycerin. Amlodipine is not associated with any adverse metabolic effects or changes in plasma lipid levels, and can therefore be used in patients with asthma, diabetes, and gout.
Patients with coronary artery disease
The efficacy of amlodipine in preventing clinical events in patients with coronary artery disease was evaluated in an independent, multicenter, randomized, double-blind, placebo-controlled trial involving 1997 patients (comparison of amlodipine to enalapril in reducing thrombosis events (CAMELOT Study)). Over 2 years, 663 patients received amlodipine at a dose of 5-10 mg, 673 patients received enalapril at a dose of 10-20 mg, and 655 patients received placebo in addition to standard therapy with statins, β-blockers, diuretics, and acetylsalicylic acid. The main efficacy results are shown in Table 1. The results indicate that treatment with amlodipine was associated with fewer hospitalizations for angina and fewer revascularization procedures in patients with coronary artery disease.
Table 1.
Number of cases of significant clinical outcomes in the CAMELOT study
| Frequency of cardiovascular events, number (%) | Amlodipine vs placebo | ||||
| Results | Amlodipine | Placebo | Enalapril | Relative risk (95% CI) | p value |
Primary endpoint Adverse cardiovascular events | 110 (16.6) | 151 (23.1) | 136 (20.0) | 0.69 (0.54-0.88) | 0.003 |
Individual components Coronary revascularization. Hospitalization for angina pectoris. Non-fatal myocardial infarction. Stroke or transient ischemic attack. Cardiovascular mortality. Hospitalization for congestive heart failure. Cardiac arrest followed by resuscitation. Peripheral vascular diseases were discovered for the first time. | 78 (11.8) 51 (17.7) 14 (2.1) 6 (0.9) 5 (0.8) 3 (0.5) 0 5 (0.8) | 103 (15.7) 84 (12.8) 19 (2.9) 12 (1.8) 2 (0.3) 5 (0.8) 4 (0.6) 2 (0.3) | 95 (14.1) 86 (12.8) 11 (1.6) 8 (1.2) 5 (0.7) 4 (0.6) 1 (0.1) 8 (1.2) | 0.73 (0.54-0.98) 0.58 (0.41-0.82) 0.73 (0.37-1.46) 0.50 (0.19-1.32) 2.46 (0.48-12.7) 0.59 (0.14-2.47) ̶ 2.6 (0.5-13.4) | 0.03 0.002 0.37 0.15 0.27 0.46 0.04 0.24 |
Use in patients with heart failure
The aim of the placebo-controlled PRAISE study was to evaluate the effect of amlodipine on the condition of patients with heart failure (NYHA functional class III-IV) who were taking digoxin, diuretics and ACE inhibitors. The study showed that the use of amlodipine did not lead to an increased risk of mortality or an increased risk of morbidity/mortality related to heart failure. PRAISE-2 is a long-term placebo-controlled study. The aim of the study was to evaluate the effect of amlodipine on patients with heart failure (NYHA functional class III-IV) without clinical symptoms or objective data confirming or underlying ischemic disease. Patients who participated in the study were taking ACE inhibitors, digitalis and diuretics for a long time. The study showed that amlodipine did not affect all-cause cardiovascular mortality. In the study, amlodipine was associated with an increased number of reports of pulmonary edema.
ALLHAT – a study of different types of treatments to prevent heart attacks
The ALLHAT (Antihypertensive and Lipid-lowering Treatment for Heart Attack Prevention) randomized, double-blind, morbidity/mortality trial was conducted in patients with mild to moderate hypertension to compare current therapeutic agents: amlodipine 2.5–10 mg/day (calcium channel blocker) or lisinopril 10–40 mg/day (ACE inhibitor) as first-line therapy and the thiazide diuretic chlorthalidone 12.5–25 mg/day.
The study included 33,357 hypertensive patients aged 55 years and older who were followed for a mean of 4.9 years. Patients had at least one additional cardiovascular risk factor, including: previous myocardial infarction or stroke >6 months before study entry or evidence of other atherosclerotic cardiovascular disease (overall 51.5%), type 2 diabetes (36.1%), dyslipidemia with high-density lipoprotein (HDL) <35 mg/dL (11.6%), left ventricular hypertrophy as determined by electrocardiogram or echocardiography (20.9%), and smoking (21.9%).
The primary endpoint was a composite of fatal CHD or nonfatal myocardial infarction. There was no statistically significant difference in the primary endpoint between amlodipine and chlorthalidone therapy: relative risk 0.98, 95% CI (0.90-1.07) p=0.65. Regarding secondary endpoints, the incidence of heart failure (component of the composite cardiovascular endpoint) was significantly higher in the amlodipine group compared with the chlorthalidone group (10.2% vs. 7.7%, relative risk 1.38, 95% CI [1.25-1.52] p<0.001). However, there was no significant difference in all-cause mortality between amlodipine-based therapy and chlorthalidone-based therapy (relative risk 0.96, 95% CI [0.89 - 1.02] p=0.20).
Properties common to perindopril and amlodipine
The ASCOT-BLPA (Anglo-Scandinavian Study of Cardiovascular Outcomes – Antihypertensive Arm) study of morbidity and mortality was conducted in 19,257 patients aged 40 to 79 years with hypertension and at least 3 of the following cardiovascular risk factors: left ventricular hypertrophy (detected by ECG or echocardiography), other abnormalities detected on ECG, type 2 diabetes mellitus, peripheral arterial disease, previous stroke or transient ischemic attack, male gender, age 55 years or older, microalbuminuria or proteinuria, smoking, plasma total cholesterol to high-density lipoprotein (HDL) cholesterol ratio of 6 or greater, and family history of early CHD. The primary objective of the study was to evaluate and compare the long-term effects of two regimens of long-term antihypertensive therapy on the combined endpoint of nonfatal myocardial infarction (including silent myocardial infarction) and fatal CHD complications, namely amlodipine in combination with perindopril, added if necessary to lower blood pressure, compared with atenolol therapy in combination with the diuretic bendroflumethiazide, added if necessary to lower blood pressure. At the end of the study, the majority of patients (78%, 14974 of 19242) were receiving at least two antihypertensive drugs and only 15% (1401 of 9634) and 9% (857 of 9608) were receiving monotherapy with amlodipine and atenolol, respectively. The study was stopped early after a median follow-up of 5.5 years by the Data Safety Monitoring Board (DSMB) because of significantly higher mortality in the atenolol-based group compared to the amlodipine group.
The study showed a non-significant reduction in the primary endpoint of non-fatal myocardial infarction (including asymptomatic myocardial infarction) and fatal coronary events by 10% in the amlodipine/perindopril group compared with the atenolol/bendroflumethiazide group. However, there was a significant reduction in all secondary endpoints (except fatal and non-fatal heart failure) in the amlodipine/perindopril group.
Endpoints:
Table 2.
| Secondary endpoints | 95% CI | p | |
| Non-fatal myocardial infarction (except asymptomatic) + fatal coronary artery disease. | 13% | 0.76‑1.00 | 0.0458 |
| Total coronary endpoint. | 13% | 0.79‑0.96 | 0.007 |
| Coronary events and interventions. | 16% | 0.78‑0.90 | <0.0001 |
| All-cause mortality. | 11% | 0.81‑0.99 | 0.0247 |
| Cardiovascular mortality. | 24% | 0.65‑0.90 | 0.0010 |
| Fatal and non-fatal stroke. | 23% | 0.66‑0.89 | 0.0003 |
| Fatal and non-fatal heart failure. | 16% | 0.66‑1.05 | 0.1257 |
Pharmacokinetics.
The rate and extent of absorption of perindopril and amlodipine, both as monodrugs and as part of the fixed combination PERINDOPRES® A, do not differ significantly.
Perindopril
Perindopril is rapidly absorbed after oral administration. Peak plasma concentrations are reached within 1 hour. The half-life of perindopril in plasma is 1 hour. Perindopril is a prodrug. 27% of the total amount of perindopril taken reaches the bloodstream as the active metabolite, perindoprilat. In addition to the active metabolite, perindoprilat, the drug forms 5 metabolites that are inactive. Peak plasma concentrations of perindoprilat are reached 3–4 hours after administration.
Food intake reduces the conversion of perindopril to perindoprilat, thus reducing its bioavailability, so the daily dose of perindopril arginine is recommended to be taken once in the morning before meals. There is a linear relationship between the dose of perindopril and its concentration in the blood plasma. The volume of distribution of unbound perindoprilat is approximately 0.2 l/kg. The binding of perindoprilat to plasma proteins is 20%, mainly with ACE, but this indicator is dose-dependent. Perindoprilat is excreted in the urine. The terminal half-life of the unbound fraction is approximately 17 hours. The steady-state plasma concentration is reached 4 days after the start of treatment.
The elimination of perindoprilat is slowed down in elderly patients and in patients with heart or renal failure (see section "Special instructions"). Therefore, routine medical supervision will include frequent monitoring of creatinine and potassium levels. Dialysis clearance of perindoprilat is 70 ml/min. The kinetics of perindopril are altered in patients with cirrhosis of the liver: the hepatic clearance of perindopril is halved. However, the amount of perindoprilat formed is not reduced. Therefore, no dose adjustment is required in such patients (see section "Special instructions").
Amlodipine
After oral administration of therapeutic doses of amlodipine, it is well absorbed and reaches maximum blood concentrations 6-12 hours after administration. Absolute bioavailability is 64 to 80%. The volume of distribution is approximately 21 l/kg. In vitro studies have shown that approximately 97.5% of circulating amlodipine is bound to plasma proteins.
Food intake does not affect the bioavailability of amlodipine. The plasma half-life is approximately 35-50 hours, which allows the drug to be administered once a day. Amlodipine is mainly metabolized in the liver to inactive metabolites. 60% of the metabolites are excreted in the urine and 10% in unchanged form.
Use in elderly patients: the time to reach the maximum concentration of amlodipine in elderly and younger patients is the same. In elderly patients, there is a tendency for amlodipine clearance to decrease and, accordingly, an increase in the area under the pharmacokinetic curve concentration-time AUC and half-life. The increase in AUC and half-life in patients with congestive heart failure was consistent with the age characteristics of the patients studied.
Use in patients with hepatic impairment: There are very limited clinical data on the use of amlodipine in patients with hepatic impairment. In patients with hepatic insufficiency, the clearance of amlodipine is reduced, resulting in a prolonged half-life and an increase in AUC by approximately 40-60%.
Indication
Arterial hypertension and/or ischemic heart disease (if treatment with perindopril and amlodipine is necessary).
Contraindication
Related to perindopril:
hypersensitivity to the active substance or to any other ACE inhibitors;
history of angioedema associated with previous treatment with ACE inhibitors;
congenital or idiopathic angioedema;
pregnancy or planning a pregnancy (see section "Use during pregnancy or breastfeeding");
simultaneous use with drugs containing the active substance aliskiren in patients with diabetes mellitus or renal insufficiency (glomerular filtration rate < 60 ml/min/1.73 m2) (see section "Interaction with other medicinal products and other types of interactions");
extracorporeal treatments that result in blood coming into contact with negatively charged surfaces (see section “Interaction with other medicinal products and other types of interactions”);
significant bilateral renal artery stenosis or stenosis of the artery to a single functioning kidney (see section "Special warnings and precautions for use").
Related to amlodipine:
severe arterial hypotension;
hypersensitivity to the active substance or to dihydropyridine derivatives;
shock, including cardiogenic shock;
obstruction of the left ventricular outflow tract (e.g. severe aortic stenosis);
heart failure after acute myocardial infarction with unstable hemodynamics.
Related to the drug PERINDOPRES® A:
All of the above contraindications associated with each of the components of the drug apply to the fixed combination PERINDOPRES® A.
Hypersensitivity to any excipient.
Interaction with other medicinal products and other types of interactions
Interactions related to perindopril
Clinical trial data suggest that dual blockade of the renin-angiotensin-aldosterone system (RAAS) through the concomitant use of ACE inhibitors, angiotensin II receptor blockers or aliskiren is associated with a higher incidence of adverse reactions such as hypotension, hyperkalaemia and decreased renal function (including acute renal failure) compared to the use of a single RAAS-acting agent (see sections 4.3 and 4.4).
Drugs that increase the risk of angioedema. Concomitant use of ACE inhibitors with sacubitril/valsartan is contraindicated as it increases the risk of angioedema. Sacubitril/valsartan should not be started earlier than 36 hours after the last dose of perindopril. Perindopril therapy should not be started earlier than 36 hours after the last dose of sacubitril/valsartan (see sections 4.3 and 4.4).
Concomitant use of ACE inhibitors with racecadotril, mTOR inhibitors (e.g. sirolimus, everolimus, temsirolimus) and gliptins (e.g. linagliptin, saxagliptin, sitagliptin, vildagliptin) may lead to an increased risk of angioedema (see section 4.4).
Drugs causing hyperkalemia. Serum potassium levels usually remain within normal limits, but hyperkalemia may occur in some patients taking PERINDOPRES® A. Some drugs or therapeutic classes of drugs may cause hyperkalemia, such as: aliskiren, potassium salts, potassium-sparing diuretics, ACE inhibitors, angiotensin II receptor antagonists, NSAIDs, heparins, immunosuppressants such as ciclosporin or tacrolimus, trimethoprim and fixed combination with sulfamethoxazole (co-trimoxazole). Concomitant use of these drugs increases the risk of hyperkalemia. Therefore, concomitant use of PERINDOPRES® A with the above-mentioned drugs is not recommended. If concomitant use of these substances is necessary, they should be used with caution and with frequent monitoring of serum potassium.
Concomitant use is contraindicated (see Contraindications section).
Aliskiren: In patients with diabetes mellitus or patients with impaired renal function, the risk of hyperkalemia, worsening of renal function, and cardiovascular morbidity and mortality is increased.
Extracorporeal therapies: Extracorporeal therapies that result in contact of blood with negatively charged surfaces, such as dialysis or hemofiltration using certain membranes with high hydraulic permeability (e.g. polyacrylonitrile) and low-density lipoprotein (LDL) apheresis using dextran sulfate, due to an increased risk of severe anaphylactoid reactions (see section 4.3). If such treatments are necessary, consideration should be given to using a different type of dialysis membrane or a different class of antihypertensive drug.
Concomitant use is not recommended (see section "Special precautions for use")
Aliskiren: In all other patients, as well as in patients with diabetes mellitus or renal impairment, the risk of hyperkalemia, worsening of renal function and cardiovascular morbidity and mortality is increased.
According to published data, in patients with established atherosclerosis, heart failure, or diabetes mellitus with target organ damage, the simultaneous use of ACE inhibitors and angiotensin receptor blockers was accompanied by an increased incidence of arterial hypotension, syncope, hyperkalemia, and deterioration of renal function (including acute renal failure) compared with monotherapy with drugs that affect the renin-angiotensin-aldosterone system (RAAS).
Estramustine: There is a risk of increased incidence of adverse reactions such as angioedema.
Potassium-sparing diuretics (e.g., triamterene, amiloride, and others), potassium salts.
Hyperkalemia (possibly fatal), especially in patients with renal insufficiency (additive hyperkalemic effect). These drugs are not recommended for concomitant use with perindopril (see section "Special warnings and precautions for use"). However, if concomitant use of these substances is necessary, they should be used with caution and with frequent monitoring of plasma potassium. Regarding the use of spironolactone in heart failure, see section "Drugs with which concomitant administration requires special attention".
Lithium: Concomitant use of lithium and ACE inhibitors is not recommended due to the possibility of a reciprocal increase in serum lithium concentrations and, consequently, an increase in its toxicity (severe neurotoxicity). However, if the need for such a combination is justified, it is recommended to monitor serum lithium concentrations (see section 4.4).
Medicinal products, concomitant administration of which requires special attention
Epidemiological studies suggest that the concomitant use of ACE inhibitors and hypoglycemic agents (insulin, oral hypoglycemic agents) may lead to an increased hypoglycemic effect with a risk of hypoglycemia. This phenomenon may occur most often in the first weeks of combined treatment and in the case of renal insufficiency.
Diuretics. In patients taking diuretics, and especially in those with impaired water and electrolyte balance, an excessive decrease in blood pressure may occur after starting treatment with an ACE inhibitor. The likelihood of developing a hypotensive effect is reduced if the diuretic is discontinued, the circulating blood volume or salt intake is increased before starting perindopril therapy, which should be started at low doses with a gradual increase. In arterial hypertension, when the previously prescribed diuretic could have caused water/electrolyte depletion, it should be discontinued before starting treatment with an ACE inhibitor (in such cases, the diuretic can be resumed over time) or the ACE inhibitor should be prescribed at a low dose with a gradual increase. In congestive heart failure on the background of taking a diuretic, ACE inhibitors should be started with the minimum dose, possibly after reducing the dose of the diuretic. In any case, it is necessary to monitor kidney function (creatinine level) during the first weeks of treatment with an ACE inhibitor.
Potassium-sparing diuretics (eplerenone, spironolactone). Special care is required when eplerenone or spironolactone at doses of 12.5 mg to 50 mg per day are used concomitantly with low doses of an ACE inhibitor. If the recommendations for the appointment of such a combination are not followed, there is a risk of hyperkalemia (possibly fatal) during the treatment of patients with NYHA class II-IV heart failure and an ejection fraction <40%, who were previously treated with an ACE inhibitor and a loop diuretic. Before prescribing such a combination, it is necessary to ensure the absence of hyperkalemia and impaired renal function. It is recommended to carefully monitor potassium and creatinine weekly during the first month of treatment and monthly thereafter.
Non-steroidal anti-inflammatory drugs (NSAIDs), including acetylsalicylic acid (≥3 g/day). A reduction in the antihypertensive effect may occur when ACE inhibitors are used concomitantly with NSAIDs, such as acetylsalicylic acid at anti-inflammatory doses, COX-2 inhibitors, non-selective NSAIDs. Concomitant use of ACE inhibitors and NSAIDs may lead to an increased risk of worsening of renal function, including the possibility of acute renal failure, and an increase in plasma potassium, especially in patients with a history of impaired renal function. This combination should be administered with caution, particularly in elderly patients. Patients should be rehydrated and renal function monitored at the start of treatment with this combination and periodically thereafter.
Drugs whose concomitant administration requires attention
Sympathomimetics may weaken the antihypertensive effect of ACE inhibitors.
Gold. Concomitant use of ACE inhibitors, including perindopril, and injectable gold (sodium aurothiomalate) may rarely result in reactions similar to those seen with nitrates (facial flushing, flushing, nausea, vomiting, and hypotension).
Interactions related to amlodipine
Concomitant use is not recommended.
Dantrolene (infusion). In experimental studies, fatal ventricular fibrillation and cardiovascular collapse have been observed in association with hyperkalemia following the administration of verapamil and dantrolene intravenously. Given the potential for hyperkalemia, it is recommended that concomitant administration of calcium antagonists such as amlodipine be avoided in patients with malignant hyperthermia or in patients suspected of having malignant hyperthermia.
CYP3A4 inducers: When used concomitantly with known CYP3A4 inducers, the plasma concentration of amlodipine may change. Therefore, blood pressure should be monitored and dose adjustments should be made during and after concomitant use with CYP3A4 inducers, particularly with strong CYP3A4 inducers (e.g. rifampicin, St. John's wort (hypericum perforatum)).
CYP3A4 inhibitors. Concomitant use of amlodipine with strong or moderate CYP3A4 inhibitors (protease inhibitors, azole antifungals, macrolides such as erythromycin or clarithromycin, verapamil or diltiazem) may result in increased amlodipine concentrations. The clinical manifestation of the above pharmacokinetic changes may be more pronounced in elderly patients. In such cases, clinical monitoring and dose adjustment are necessary. There is an increased risk of arterial hypotension in patients taking clarithromycin in combination with amlodipine. Close observation is recommended in such patients.
Drugs whose concomitant administration requires attention
When amlodipine is used with other drugs with antihypertensive properties, an additive antihypertensive effect is possible.
Tacrolimus: There is a risk of increased blood levels of tacrolimus when co-administered with amlodipine. To avoid toxic effects of tacrolimus, blood levels should be monitored and, if necessary, the dose adjusted in patients receiving amlodipine.
Mechanistic target of rapamycin (mTOR) inhibitors. The mTOR inhibitors, sirolimus, temsirolimus, and everolimus, are substrates of CYP3A. Amlodipine is a weak CYP3A inhibitor. When co-administered with mTOR inhibitors, amlodipine may increase the concentration of mTOR inhibitors.
Cyclosporine. No interaction studies have been conducted with cyclosporine and amlodipine in healthy volunteers or other subjects. The exception is renal transplant patients, in whom cyclosporine concentrations fluctuated with an average increase of 0 to 40%. In renal transplant patients receiving amlodipine and cyclosporine, cyclosporine blood levels should be monitored and the cyclosporine dose reduced if necessary.
Simvastatin: Coadministration of amlodipine in multiples of 10 mg with simvastatin 80 mg resulted in a 77% increase in simvastatin concentrations compared to simvastatin alone. Patients should limit their simvastatin dose to 20 mg daily.
Other combinations
Clinical interaction studies have shown that amlodipine does not affect the pharmacokinetics of atorvastatin, digoxin, and warfarin.
It is not recommended to use amlodipine with grapefruit or grapefruit juice, as bioavailability may increase in some patients, leading to increased hypotensive effect.
Interactions associated with the fixed combination PERINDOPRES® A
Medicinal products, the simultaneous use of which requires special caution
Baclofen enhances the antihypertensive effect. It is necessary to monitor blood pressure and kidney function, and if necessary, adjust the dose.
Medicines, concomitant administration of which requires attention
Antihypertensives (such as ß-blockers) and vasodilators:
Concomitant use of these agents may enhance the hypotensive effect of perindopril and amlodipine.
Concomitant use with nitroglycerin and other nitrates or with other vasodilators may cause a further decrease in blood pressure and should therefore be administered with caution.
Corticosteroids, tetracosactide: weakening of the antihypertensive effect (due to water and salt retention by corticosteroids).
Alpha-blockers (prazosin, alfuzosin, doxazosin, tamsulosin, terazosin): enhance the antihypertensive effect and increase the risk of orthostatic hypotension.
Amifostine: may increase the risk of
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.