Qlaira tablets combination pack No. 28
Instructions for Qlaira tablets combination pack No. 28
Composition
active ingredients: estradiol valerate, dienogest;
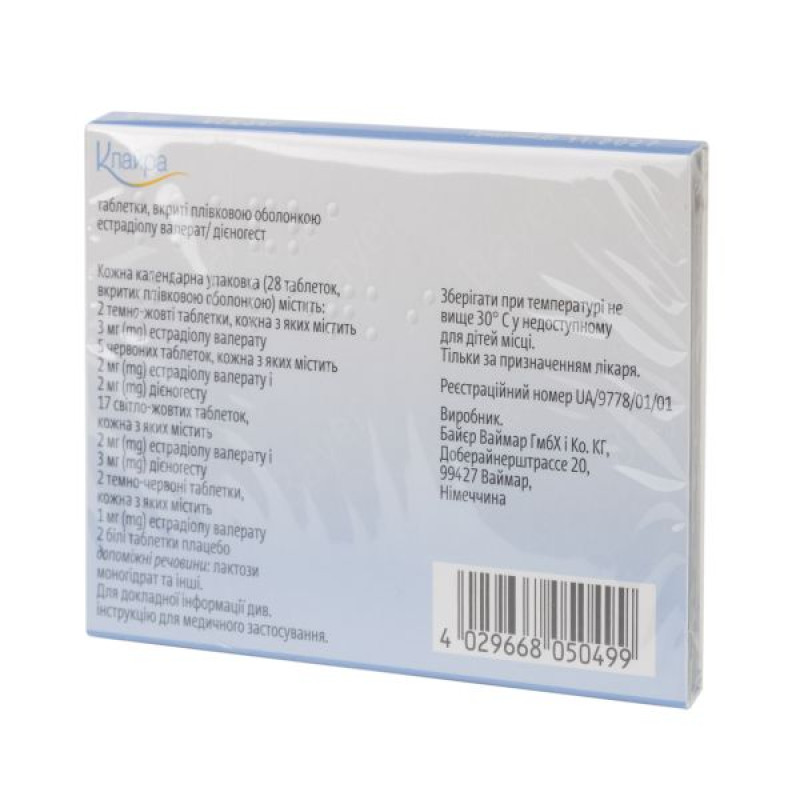
Each calendar pack (28 film-coated tablets) contains:
2 dark yellow tablets, each containing 3 mg of estradiol valerate;
5 red tablets, each containing 2 mg of estradiol valerate and 2 mg of dienogest;
17 light yellow tablets, each containing 2 mg of estradiol valerate and 3 mg of dienogest;
2 dark red tablets, each containing 1 mg of estradiol valerate;
2 white placebo pills;
excipients: lactose monohydrate, corn starch, pregelatinized starch, povidone, magnesium stearate, hypromellose, macrogol 6000, talc, titanium dioxide (E 171), yellow iron oxide (E 172) or red iron oxide (E 172);
placebo: lactose monohydrate, corn starch, povidone, magnesium stearate, hypromellose, talc, titanium dioxide (E 171).
Dosage form
Film-coated tablets.
Main physicochemical properties: round biconvex tablets, film-coated, dark yellow, dark red, light yellow, red and white, on one side of which the letters "DD", "DJ", "DH", "DN" or "DT" are embossed, respectively, in a regular hexagon.
Pharmacotherapeutic group
Sex hormones and drugs used in pathologies of the genital area. Hormonal contraceptives for systemic use. ATX code G03A B08.
Pharmacological properties
Pharmacodynamics
In clinical studies conducted with Qlaira in the European Union and in the USA/Canada, the following Pearl indices were determined:
Pearl Index (patient age 18–50 years):
Method uncertainty: 0.42 (upper limit of the 95% confidence interval (CI) 0.77).
Patient error and method unreliability: 0.79 (upper limit of 95% CI 1.23).
Pearl Index (patient age 18–35 years):
method uncertainty: 0.51 (upper limit of 95% CI 0.97).
Patient error and method unreliability: 1.01 (upper limit of 95% CI 1.59).
The contraceptive effect of combined oral contraceptives (COCs) is based on the interaction of various factors, the most important of which are the suppression of ovulation, changes in cervical secretions, and changes in the endometrium.
The Qlaira treatment regimen (a gradual reduction in estrogen and a gradual increase in progestogen) can be used to treat heavy menstrual bleeding (MMB) in women without organic pathology, sometimes called dysfunctional uterine bleeding (DUB).
Two multicenter, randomized, double-blind studies with a similar design were conducted to investigate the efficacy and safety of Qlaira in women with symptoms of PMS who wished to use oral contraception. A total of 269 women were randomized to Qlaira and 152 to placebo.
After 6 months of therapy, the average amount of blood lost during menstruation decreased by 88% (from 142 ml to 17 ml) in the Qlaira group and by 24% (from 154 ml to 117 ml) in the placebo group.
The number of women who had complete resolution of their PMS symptoms after 6 months of therapy was 29% in the Qlaira group and 2% in the placebo group.
The estrogen contained in Qlaira is estradiol valerate, an ester of 17-beta-estradiol, a natural human hormone (1 mg of estradiol valerate corresponds to 0.76 mg of 17-beta-estradiol). This estrogen differs from estrogens such as ethinyl estradiol or its precursor mestranol, which are part of other COCs, in the absence of an ethinyl group in the 17-alpha position.
Dienogest is a nortestosterone derivative characterized by the absence of androgenic activity and the presence of an antiandrogenic effect, which is approximately one third of the action of cyproterone acetate. Dienogest binds to progesterone receptors in the female uterus, while showing only 10% of the relative affinity for progesterone. Despite the low affinity for progesterone receptors, dienogest demonstrates a potent progestogenic effect in vivo. Dienogest does not exhibit significant androgenic, mineralocorticoid or glucocorticoid properties in vivo.
Histological examination of the endometrium performed in a subgroup of women (n = 218) in a clinical trial after 20 treatment cycles revealed no abnormalities.
Pharmacokinetics
Dienogest
Distribution. A fairly significant part of circulating dienogest (10%) is in free form, and about 90% is nonspecifically bound to albumin. Dienogest does not bind to specific transport proteins - sex hormone binding globulin (SHBG) and corticosteroid binding globulin (CBG). After intravenous administration of 85 μg 3H-dienogest, the volume of distribution of dienogest at steady state (Vd,ss) is 46 l.
Metabolism: Dienogest is almost completely metabolized by the known pathways of steroid hormone metabolism (hydroxylation, conjugation), mainly by CYP3A4. Pharmacologically inactive metabolites are rapidly eliminated from plasma, resulting in dienogest as the major fraction in plasma accounting for approximately 50% of circulating dienogest derivatives. Total clearance after intravenous administration of 3H-dienogest is 5.1 l/h.
Excretion. The half-life of dienogest from blood plasma is about 11 hours. Dienogest is very actively metabolized and only 1% of the active substance is excreted unchanged. After oral administration of dienogest at a dose of 0.1 mg/kg, the drug is excreted by the kidneys and through the intestines in a ratio of approximately 3:1. When taken orally, 42% of the dose is excreted during the first 24 hours, and 63% - within 6 days by renal excretion. After 6 days, a total of 86% of the administered dose is excreted in the urine and feces.
Steady state. The pharmacokinetics of dienogest are independent of the level of GH. The steady-state concentration of dienogest is achieved after 3 days of administration of the same dose of 3 mg dienogest in combination with 2 mg estradiol valerate. The minimum, maximum and average concentrations of dienogest in serum at steady state are 11.8 ng/ml, 82.9 ng/ml and 33.7 ng/ml, respectively. The average accumulation coefficient, taking into account the AUC data (0-24 h), is 1.24.
Estradiol valerate
Absorption. When estradiol valerate is administered orally, it is completely absorbed. The cleavage into estradiol and valeric acid occurs during absorption into the gastrointestinal mucosa or during the first pass through the liver. As a result, estradiol and its metabolites: estrone and estriol are formed. After a single dose of a tablet containing 3 mg of estradiol valerate, on the 1st day, the maximum concentration of estradiol in the blood serum, which is 70.6 pg/ml, is reached after 1.5–12 hours.
Metabolism. Valeric acid is very rapidly metabolized. After oral administration, about 3% of the dose is directly available as estradiol. Estradiol undergoes extensive first-pass metabolism in the liver and a significant part of the dose is metabolized in the gastrointestinal mucosa. Together with presystemic metabolism in the liver, about 95% of the oral dose is metabolized before reaching the systemic circulation. The main metabolites are estrone, estrone sulfate and estrone glucuronide.
Distribution. In serum, 38% of estradiol is bound to GH, 60% to albumin; and 2–3% circulates unchanged. Estradiol may cause (depending on the dose) a slight increase in serum GH. On day 21 of treatment, GH was approximately 148% of baseline, and on day 28 (end of the placebo period), this had decreased to approximately 141% of baseline. After intravenous administration, the apparent volume of distribution was approximately 1.2 L/kg.
Elimination. The plasma half-life of circulating estradiol is about 90 minutes. However, the situation is somewhat different after oral administration. Due to the large number of circulating estrogen sulfates and glucuronides and enterohepatic recirculation, the terminal half-life of estradiol after oral administration is a complex parameter that depends on all the processes mentioned and ranges from 13 to 20 hours. Estradiol and its metabolites are mainly excreted in the urine, about 10% is excreted in the feces.
Steady state. The pharmacokinetics of estradiol are influenced by the level of GH. In young women, the measured concentration of estradiol in the blood plasma consists of endogenous estradiol and estradiol that entered the body with the drug Qlaira. During the phase of taking tablets containing 2 mg estradiol valerate + 3 mg dienogest, the maximum and average concentration of estradiol in the blood serum at steady state were 66.0 pg/ml and 51.6 pg/ml, respectively. Stable trough concentrations of estradiol were maintained throughout the 28-day cycle in the range of 28.7 pg/ml to 64.7 pg/ml.
Special categories of patients
The pharmacokinetics of Qlaira have not been studied in patients with hepatic or renal impairment.
Preclinical safety data
Preclinical data obtained from conventional studies of toxicity, genotoxicity and reproductive toxicity with repeated administration of the drug indicate no specific risk for humans. In a study of carcinogenic potential with dienogest in animals, no increase in tumors was observed. However, it is known that sex steroid hormones, due to their hormonal activity, can promote the growth of certain hormone-dependent tissues and tumors.
Indication
Oral contraception.
Treatment of heavy menstrual bleeding in women without organic pathology who are prescribed oral contraception.
Contraindication
You should not use CHCs if you have any of the conditions listed below. If any of these develop for the first time during CHC use, you should stop taking the drug immediately.
Presence or risk of venous thromboembolism (VTE):
current (while on anticoagulant therapy) or history of venous thromboembolism (e.g. deep vein thrombosis (DVT), pulmonary embolism (PE); known hereditary or acquired predisposition to venous thromboembolism, such as resistance to activated protein C (including factor V Leiden mutation), antithrombin-III deficiency, protein C deficiency, protein S deficiency;
major surgical interventions with prolonged immobilization (see section "Special instructions for use");
high risk of venous thromboembolism due to the presence of multiple risk factors (see section "Special warnings and precautions for use").
Presence or risk of arterial thromboembolism (ATE):
Arterial thromboembolism: current or history of arterial thromboembolism (e.g. myocardial infarction) or presence of prodromal symptoms (e.g. angina); cerebrovascular accident: current or history of stroke, presence of prodromal symptoms (e.g. transient ischemic attack (TIA)); known hereditary or acquired predisposition to arterial thromboembolism, such as hyperhomocysteinemia and antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant); history of migraine with focal neurological symptoms;
high risk of arterial thromboembolism due to the presence of multiple risk factors (see section "Special warnings and precautions for use") or due to the presence of one serious risk factor, such as:
- diabetes mellitus with vascular complications;
- severe arterial hypertension;
- severe dyslipoproteinemia;
Current or history of severe liver disease, until liver function tests have returned to normal.
Benign or malignant liver tumor present or in the past.
Known or suspected malignant tumors (e.g., genital or mammary) that are sex hormone-dependent.
Vaginal bleeding of unknown etiology.
Hypersensitivity to the active substances or to any of the components of the drug.
Interaction with other medicinal products and other types of interactions
The information for the concomitant medicinal product should be consulted to identify potential interactions.
Interaction studies have only been conducted in adult patients.
Information on the types of interactions listed below is taken from publications on COCs in general or from clinical trial results with Qlaira.
The effect of other medicines on Qlaira.
Interactions with other medications may result in breakthrough bleeding and/or decreased effectiveness of hormonal contraceptives.
Therapy.
Enzyme induction may occur within a few days of treatment. Maximal enzyme induction is usually observed only after a few weeks, but may persist for 4 weeks or more after discontinuation of the drug.
Short-term therapy.
During short-term treatment with enzyme-inducing drugs, a woman should use a barrier method or another method of contraception in addition to COCs.
A barrier method of contraception should be used throughout the entire period of combined therapy and for 28 days after its discontinuation. If therapy extends beyond the period of taking active COC tablets, placebo tablets should not be taken, but the next COC pack should be started immediately.
Long-term therapy
Women who need to receive long-term therapy with liver enzyme-inducing agents are advised to use another reliable non-hormonal method of contraception.
Drugs that increase the clearance of COCs (reduced efficacy of COCs by enzyme induction): barbiturates, bosentan, carbamazepine, phenytoin, primidone, rifampicin; drugs for the treatment of HIV, including ritonavir, nevirapine and efavirenz; and possibly also felbamate, griseofulvin, oxcarbazepine, topiramate and drugs containing St. John's wort (Hypericum perforatum).
In a clinical study, rifampicin, a potent inducer of cytochrome P450 CYP 3A4, significantly reduced the steady-state concentrations and systemic exposure of dienogest and estradiol. The systemic exposure of dienogest and estradiol at steady state, as determined by AUC (0-24 hours), was reduced by 83% and 44%, respectively.
Drugs with variable effects on COC clearance
Concomitant use of COCs, many combinations of HIV protease inhibitors and non-nucleoside reverse transcriptase inhibitors, including combinations with hepatitis C virus (HCV) inhibitors, may result in increased or decreased plasma concentrations of estrogen or progestins. The cumulative effect of these changes may be clinically significant in some cases.
Drugs that reduce COC clearance (enzyme inhibitors)
Dienogest is a substrate of cytochrome CYP3A4.
The clinical significance of potential interactions with enzyme inhibitors is unknown.
Concomitant use of strong CYP3A4 inhibitors may lead to increased plasma concentrations of estrogen or progestin, or both.
Concomitant use of ketoconazole, a potent CYP3A4 inhibitor, resulted in a 2.9-fold increase in steady-state AUC (0–24 hours) for dienogest and a 1.6-fold increase in estradiol.
With simultaneous use of erythromycin, which is a moderate inhibitor, an increase in AUC (0-24 hours) at steady state for dienogest and estradiol was observed by 1.6 and 1.3 times, respectively. The clinical significance of these interactions is unknown.
The effect of Qlaira on other medicines
Oral hormonal contraceptives may affect the metabolism of certain other drugs. Accordingly, plasma and tissue concentrations may increase (e.g., cyclosporine) or decrease (e.g., lamotrigine).
No effect on the pharmacokinetics of nifedipine was observed when it was co-administered with 2 mg dienogest and 0.03 mg ethinylestradiol, which confirms the results of in vitro studies, according to which inhibition of CYP enzymes by Qlaira when taken in therapeutic doses is unlikely.
Other types of interactions
Laboratory tests
The use of contraceptive steroids may affect the results of some laboratory tests, including biochemical parameters of liver, thyroid, adrenal and renal function, plasma levels of proteins (carriers) such as sex hormone binding globulin, lipid/lipoprotein fractions, parameters of carbohydrate metabolism, as well as coagulation and fibrinolysis. Such changes are usually within the limits of laboratory norms.
Application features
The decision to prescribe Qlaira should take into account the individual risk factors, including risk factors for venous thromboembolism (VTE), as well as the risk of VTE associated with Qlaira compared with other combined hormonal contraceptives (CHCs) (see sections “Contraindications” and “Special warnings and precautions for use”).
Warning
If any of the following conditions or risk factors are present, the appropriateness of using Qlaira should be discussed with the woman.
If any of the following conditions or risk factors worsen or occur for the first time, the woman should consult her doctor. The doctor will then decide whether to stop taking Qlaira.
In case of suspected or confirmed VTE or ATE, CHC use should be discontinued. If anticoagulant therapy is initiated, alternative adequate contraception should be provided due to the teratogenic effects of anticoagulants (coumarins).
The following warnings and precautions for use are based on clinical and epidemiological data on COCs containing ethinylestradiol.
Circulatory disorders
Risk of developing venous thromboembolism (VTE)
The use of any CHC increases the risk of VTE in women who use it compared with those who do not use it. Products containing levonorgestrel, norgestimate or norethisterone are associated with the lowest risk of VTE. Limited data suggest that the risk of VTE may be comparable with Qlaira. The decision to use any product other than Qlaira, other than the product with the lowest risk of VTE, should only be made after discussion with the woman. She should be made sure that she is aware of the risk of VTE associated with CHC use, the extent of her existing risk factors and the fact that the risk of VTE is highest during the first year of use. Some data suggest that the risk of VTE may increase when CHC use is resumed after a break of 4 weeks or longer.
About 2 in 10,000 women who are not using CHCs and are not pregnant will develop a VTE in 1 year. However, the risk for an individual woman may be much higher depending on the risk factors she has (see below).
According to epidemiological studies involving women using low-dose (–12 people develop VTE within one year.
It is estimated that out of 10,000 women who use a CHC containing levonorgestrel, about 61 will develop a VTE in one year.
1 On average 5–7 cases per 10,000 women-years, based on a calculation of the relative risk for women using levonorgestrel-containing CHCs compared to women not using CHCs (approximately 2.3–3.6 cases).
Limited epidemiological data suggest that the risk of VTE with Qlaira may be similar to that with other CHCs containing levonorgestrel.
The number of VTE cases per year was lower than expected during pregnancy or in the postpartum period.
VTE can be fatal in 1–2% of cases.
Thrombosis in other blood vessels, such as the arteries and veins of the liver, kidneys, mesenteric vessels, retinal veins and arteries, has been reported extremely rarely in women using CHCs.
The risk of developing venous thromboembolic complications in women using CHCs may be significantly higher in the presence of additional risk factors, especially multiple ones (see Table 1).
Qlaira is contraindicated in women with multiple risk factors that may increase the risk of venous thrombosis (see section 4.3). If a woman has more than one risk factor, the increased risk may be greater than the sum of the risks associated with each individual factor, so the overall risk of VTE should be considered. If the benefit/risk ratio is unfavourable, CHCs should not be prescribed (see section 4.3).
Table 1
Risk factors for developing VTE
| Risk factor | Note |
| Obesity (body mass index exceeds 30 kg/m2). | The risk increases significantly with increasing body mass index. It is especially important to pay attention to the presence of other risk factors. |
Prolonged immobilization, major surgery, any surgery on the lower extremities or pelvic organs, neurosurgery, or extensive trauma. Note: Temporary immobilization, including flights > 4 hours, may also be a risk factor for VTE, especially in women with other risk factors. | In such situations, it is recommended to discontinue use of the drug (in the case of elective surgery at least 4 weeks in advance) and not resume use earlier than 2 weeks after full recovery of motor activity. In order to avoid unwanted pregnancy, other methods of contraception should be used. Antithrombotic therapy should be considered if Qlaira has not been discontinued beforehand. |
| Family history (venous thromboembolism in a relative or parent, especially at a relatively young age, for example under 50 years of age). | If a hereditary predisposition is suspected, women are advised to consult a specialist before using any CHC. |
| Other conditions associated with VTE. | Cancer, systemic lupus erythematosus, hemolytic uremic syndrome, chronic inflammatory bowel disease (Crohn's disease or ulcerative colitis), and sickle cell anemia. |
| Age. | Especially over the age of 35. |
There is no consensus on the possible influence of varicose veins and superficial thrombophlebitis on the onset or development of venous thrombosis.
Attention should be paid to the increased risk of thromboembolism during pregnancy and in the postpartum period, especially within 6 weeks after delivery (for information on pregnancy and lactation, see section "Use during pregnancy or breastfeeding").
Symptoms of VTE (deep vein thrombosis and pulmonary embolism)
Women should be advised to contact their doctor immediately if they experience the following symptoms and to inform them that they are using CHCs.
Symptoms of DVT may include:
- unilateral swelling of the thigh, lower leg and/or foot or swelling along a vein;
- pain or increased sensitivity in the leg that can only be felt while standing or walking;
- increased sensation of warmth in the affected leg, redness or discoloration of the skin of the lower limb.
Symptoms of pulmonary embolism (PE) may include:
- sudden shortness of breath of unknown origin or rapid breathing;
- sudden cough, which may be accompanied by hemoptysis;
- sharp pain in the chest;
- dizziness;
- fast or irregular heartbeat.
Some of these symptoms (e.g., shortness of breath, cough) are nonspecific and may be misinterpreted as more common or less serious conditions (e.g., respiratory tract infections).
Other signs of vascular occlusion may include sudden pain, swelling, and slight blueness of the limb.
When the vessels of the eye are blocked, symptoms may include blurred vision, which is not accompanied by pain and can progress to vision loss. Sometimes vision loss develops almost instantly.
Risk of developing arterial thromboembolism (ATE)
Epidemiological studies have shown that the use of any CHC is associated with an increased risk of ATE (myocardial infarction) or cerebrovascular events (transient ischemic attack, stroke). Arterial thromboembolic events can be fatal.
Risk factors for developing ATE
The risk of arterial thromboembolic complications or cerebrovascular events is increased in women with risk factors when using CHCs (see Table 2). Qlaira is contraindicated if women have one serious or multiple risk factors for ATE that may increase their risk of arterial thrombosis (see section 4.3). If a woman has more than one risk factor, the increased risk may be greater than the sum of the risks associated with each individual factor, so the overall risk should be considered. If the benefit/risk ratio is unfavourable, CHCs should not be prescribed (see section 4.3).
Table 2
Risk factors for developing ATE
| Risk factor | Note |
| Increasing age. | Especially over the age of 35. |
| Smoking. | Women using CHCs are advised to abstain from smoking. Women aged 35 years and over who continue to smoke are strongly advised to use another method of contraception. | Arterial hypertension. |
| Obesity (body mass index exceeds 30 kg/m2). | The risk increases significantly with increasing body mass index. This is especially important if women have other risk factors. |
| Family history (arterial thromboembolism in a relative or parent, especially at a relatively young age, for example under 50 years of age). | If a hereditary predisposition is suspected, women are advised to consult a specialist before using any CHC. |
| Migraine. | An increase in the frequency or severity of migraine during CHC use (possible prodromal states before the development of cerebrovascular events) may be a reason for immediate discontinuation of CHC use. |
| Other conditions associated with adverse vascular reactions. | Diabetes mellitus, hyperhomocysteinemia, heart valve defects, atrial fibrillation, dyslipoproteinemia, and systemic lupus erythematosus. |
Symptoms of ATE
Women should be advised to contact their doctor immediately if they experience the following symptoms and to inform them that they are using CHCs.
Symptoms of cerebral circulation disorders may include:
- sudden numbness or weakness of the muscles of the face, arms or legs, especially on one side of the body;
- sudden difficulty walking, dizziness, loss of balance or coordination;
- sudden confusion, problems with speech or understanding language;
- sudden vision loss in one or both eyes, sudden, severe or prolonged headache without an apparent cause;
- loss of consciousness or fainting with or without an epileptic seizure.
The transient nature of the symptoms may indicate a transient ischemic attack.
Symptoms of myocardial infarction may include:
- pain, discomfort, pressure, feeling of heaviness, squeezing or fullness in the chest, arm or behind the breastbone;
- pain that may radiate to the back, jaw, throat, arm, stomach;
- feeling of fullness, indigestion and shortness of breath;
- sweating, nausea, vomiting or dizziness;
- severe weakness, anxiety, shortness of breath, rapid or irregular heartbeat.
Tumors
Some epidemiological studies have shown that long-term use of COCs (>5 years) may increase the risk of cervical cancer, but this statement is still controversial, as it is not yet clear to what extent the results of the studies took into account concomitant factors, such as sexual behavior or the presence of human papillomavirus infection.
A meta-analysis of 54 epidemiological studies has shown a small increased relative risk (RR = 1.24) of breast cancer in women who use COCs. This increased risk gradually disappears within 10 years after stopping COCs. Since breast cancer is rare in women under 40 years of age, the increase in breast cancer in women who are current or recent users of COCs is small compared with the overall risk of breast cancer. The results of these studies do not provide evidence of a causal relationship. The observed increased risk may be due to earlier diagnosis of breast cancer in women who use COCs, to the biological effects of COCs, or to a combination of both. It has been noted that breast cancer found in women who have ever used COCs is usually clinically less severe than in women who have never used COCs.
In isolated cases, benign and, even more rarely, malignant liver tumors have been observed in women using COCs. In some cases, such tumors have led to life-threatening intra-abdominal bleeding. In cases of severe upper abdominal pain, liver enlargement or signs of intra-abdominal bleeding in women using COCs, a liver tumor should be considered in the differential diagnosis.
Other states
Women with hypertriglyceridemia or a family history of this condition may be at increased risk of developing pancreatitis when using COCs.
Although a slight increase in blood pressure has been reported in many women using COCs, clinically significant increases are rare. However, if persistent clinically significant hypertension develops during COC use, the physician should discontinue COCs and initiate treatment for the hypertension. If blood pressure returns to normal after antihypertensive therapy, COC use may be resumed if deemed appropriate.
The following conditions have been reported to occur or worsen during pregnancy and COC use, but the relationship between the two conditions and COC use has not been conclusively proven: jaundice and/or pruritus associated with cholestasis; gallstone formation; porphyria; systemic lupus erythematosus; haemolytic-uraemic syndrome; Sydenham's chorea; herpes gestationis; hearing loss associated with otosclerosis.
In women with hereditary angioedema, exogenous estrogens may induce or exacerbate symptoms of the disease.
COCs may also affect peripheral insulin resistance and glucose tolerance, but to date there is no evidence to suggest that a change in therapeutic regimen is necessary in patients with diabetes who use low-dose COCs (containing the drug.
Worsening of endogenous depression, epilepsy, Crohn's disease and ulcerative colitis has been reported during COC use.
Depressed mood and depression are well-known side effects that can occur with hormonal contraceptives (see section 4.8). Depression can be a serious condition and is a well-known risk factor for suicidal behaviour and suicide. Women should be advised to seek medical advice if they experience mood changes or symptoms of depression, including shortly after starting treatment.
Chloasma may occasionally occur, especially in women with a history of chloasma during pregnancy. Women with a tendency to chloasma should avoid exposure to the sun or ultraviolet radiation while taking COCs.
Estrogens may cause fluid retention, therefore patients with cardiac disorders or impaired renal function should be closely monitored. Special attention should be paid to patients with end-stage renal disease due to the possibility of increased plasma estrogen concentrations after use of Qlaira.
One tablet of Qlaira contains no more than 50 mg of lactose. Patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or glucose-galactose malabsorption who are on a lactose-free diet are advised to take this amount of lactose into account.
Medical examination/consultation
Before initiating or reinstituting Qlaira, a complete medical history (including family history) should be taken and pregnancy should be excluded. Blood pressure should be measured and the patient should be examined, taking into account the contraindications (see section 4.3) and precautions (see section 4.4). The woman should be advised of the information on venous and arterial thrombosis, including the risk associated with Qlaira compared with other CHCs, the symptoms of VTE and ATE, known risk factors and the actions to be taken if thrombosis is suspected.
The woman should also be aware that she should carefully read the instructions for medical use of the medicinal product and follow the recommendations given therein. The frequency and nature of examinations should be based on existing standards of medical practice and take into account the individual characteristics of each woman.
Women should be informed that oral contraceptives do not protect against HIV infection (AIDS) and other sexually transmitted diseases.
Decreased efficiency
The effectiveness of COCs may be reduced, for example, in the event of missing a hormone-containing pill (see section "Method of administration and dosage"), gastrointestinal disorders (see section "Method of administration and dosage") during the use of hormone-containing pills or concomitant therapy (see section "Interaction with other medicinal products and other types of interactions").
Cycle control
When using all COCs, irregular bleeding (spotting or breakthrough bleeding) may occur, especially during the first months of use.
Therefore, evaluation of any irregular bleeding is important after an adaptation period of about 3
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.