Raft Dexamethasone solution for injection 4 mg/ml ampoule 2 ml No. 10
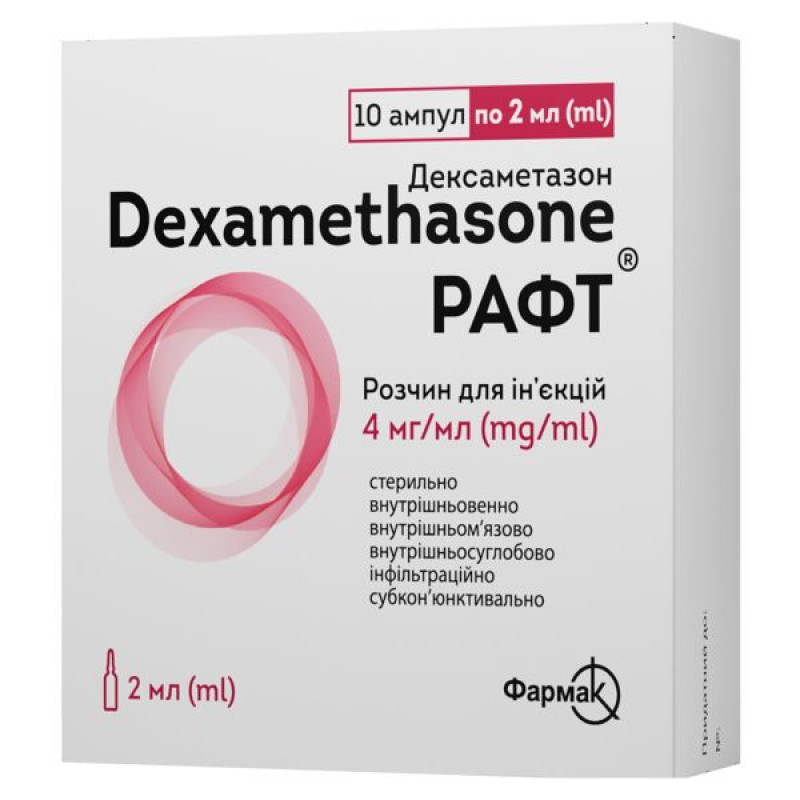
Instructions Raft Dexamethasone solution for injection 4 mg/ml ampoule 2 ml No. 10
Composition
active ingredient: dexamethasone sodium phosphate;
1 ml of solution contains dexamethasone sodium phosphate in terms of dexamethasone phosphate – 4 mg;
Excipients: disodium edetate, sodium citrate, creatinine, 1 M sodium hydroxide solution, water for injections.
Dosage form
Solution for injection.
Main physicochemical properties: at the time of release: clear colorless liquid; during the shelf life: clear colorless or yellowish liquid.
Pharmacotherapeutic group
Glucocorticosteroids. ATX code H02A B02.
Pharmacological properties
Pharmacodynamics
Dexamethasone is a monofluorinated glucocorticoid with pronounced antiallergic, anti-inflammatory, and membrane-stabilizing properties, which also affects carbohydrate, protein, and fat metabolism.
Dexamethasone has a glucocorticoid effect, which is almost 7.5 times higher than that of prednisolone and prednisone, when compared with hydrocortisone, the effectiveness of dexamethasone is 30 times higher, while there are no mineralocorticoid effects. Glucocorticoids such as dexamethasone exert their biological effect by activating the transcription of genes sensitive to corticoids. Anti-inflammatory, immunosuppressive and antiproliferative effects are also due to a decrease in the formation, release and activity of inflammatory mediators and inhibition of specific functions and migration of inflammatory cells. In addition, corticosteroids can inhibit the action of sensitized T-lymphocytes and macrophages on target cells.
If long-term use of corticosteroids is necessary, the possible induction of transit insufficiency of the adrenal cortex should be taken into account. The risk of suppression of the hypothalamic-pituitary-adrenal cortex system depends, among other things, on individual factors.
Clinical efficacy and safety - COVID-19
Clinical efficacy
RECOVERY (Randomised Evaluation of Covid-19 Therapy)1 is an investigator-initiated, individually randomised, controlled, open-label, adaptive platform trial to assess the effects of potential treatments in patients hospitalised with COVID-19.
The trial was conducted in 176 hospitals in the UK. 6425 patients were randomised to receive dexamethasone (2104 patients) or usual care (4321 patients). 89% of patients had laboratory-confirmed SARS-CoV-2 infection.
At randomization, 16% of patients received invasive mechanical ventilation (VMV) or extracorporeal membrane oxygenation, 60% received oxygen alone (with or without noninvasive ventilation), and 24% received neither.
The mean age of the patients was 66.1 ± 15.7 years. 36% of the patients were female. 24% of the patients had a history of diabetes, 27% had heart disease, and 21% had chronic lung disease.
Primary endpoint
Mortality at day 28 was significantly lower in the dexamethasone group than in the usual care group, where mortality was reported in 482 of 2104 patients (22.9%) and 1110 of 4321 patients (25.7%), respectively (rate ratio, 0.83; 95% confidence interval (CI), 0.75-0.93; P < 0.001).
In the dexamethasone group, the incidence of fatal outcomes was lower among patients in the usual care group receiving invasive mechanical ventilation (29.3% vs. 41.4%; rate ratio, 0.64; 95% CI, 0.51-0.81) and among those receiving supplemental oxygen without invasive mechanical ventilation (23.3% vs. 26.2%; rate ratio, 0.82; 95% CI, 0.72-0.94).
There was no clear effect of dexamethasone among patients who were not receiving any respiratory support at randomization (17.8% vs. 14.0%; rate ratio, 1.19; 95% CI, 0.91-1.55).
Secondary endpoint
Patients in the dexamethasone group had a shorter length of hospital stay than those in the usual care group (median, 12 days vs. 13 days) and were more likely to be discharged from the hospital within 28 days (rate ratio, 1.10; 95% CI, 1.03-1.17).
According to the primary endpoint, the greatest effect in reducing the length of hospital stay to 28 days was observed among patients receiving invasive mechanical ventilation at randomization (rate ratio, 1.48; 95% CI, 1.16, 1.90), followed by patients receiving oxygen alone (rate ratio, 1.15; 95% CI, 1.06-1.24), and no beneficial effect in patients not receiving oxygen (rate ratio, 0.96; 95% CI, 0.85-1.08).
| Result | Dexamethasone | Conventional treatment | Risk frequency coefficient* |
| (N = 2104) | (N = 4321) | (95% CI) | |
| Number/total number of patients (%) | |||
| Primary endpoint | 482/2104 (22.9) | 1110/4321 (25.7) | 0.83 (0.75-0.93) |
| Mortality within 28 days | |||
| Secondary endpoint | |||
| Discharged from hospital within 28 days | 1413/2104 (67.2) | 2745/4321 (63.5) | 1.10 (1.03-1.17) |
| Invasive mechanical ventilation or fatal outcome†: | 456/1780 (25.6) | 994/3638 (27.3) | 0.92 (0.84-1.01) |
| – invasive mechanical ventilation | 102/1780 (5.7) | 285/3638 (7.8) | 0.77 (0.62-0.95) |
| – fatal outcome | 387/1780 (21.7) | 827/3638 (22.7) | 0.93 (0.84-1.03) |
| Dexamethasone | Routine care | RR (95% Cl) | |
| Lack of oxygen (x | 2 | = 0.70; p=0.40) | |
| 1 | |||
| 10/197 (5.1%) | 18/462 (3.9%) | 1.31 (0.60-2.83) | |
| ≥ 70 | 25/114 (21.9%) | 35/224 (15.6%) | 1.46 (0.88-2.45) |
| ≥ 80 | 54/190 (28.4%) | 92/348 (26.4%) | 1.06 (0.76-1.49) |
| Subtotal | 89/501 (17.8%) | 145/1034 (14.0%) | 1.19 (0.91-1.55) |
| Oxygen only (x | 2 | = 2.54; p=0.11) | |
| 1 | |||
| 53/675 (7.9%) | 193/1473 (13.1%) | 0.58 (0.43-0.78) | |
| ≥ 70 | 104/306 (34.0%) | 178/531 (33.5%) | 0.98 (0.77-1.25) |
| ≥ 80 | 141/298 (47.3%) | 311/600 (51.8%) | 0.85 (0.70-1.04) |
| Subtotal | 298/1279 (23.3%) | 682/2604 (26.2%) | 0.82 (0.72-0.94) |
| Mechanical ventilation (x | 2 | = 0.28; p=0.60) | |
| 1 | |||
| 66/269 (24.5%) | 217/569 (38.1%) | 0.61 (0.46-0.81) | |
| ≥ 70 | 26/49 (53.1%) | 58/104 (55.8%) | 0.85 (0.53-1.34) |
| ≥ 80 | 3/6 (50.0%) | 8/10 (80.0%) | 0.39 (0.10-1.47) |
| Subtotal | 95/324 (29.3%) | 283/683 (41.4%) | 0.64 (0.51-0.81) |
| All participants | 482/2104 (22.9%) | 1110/4321 (25.7%) | 0.83 (0.75-0.93) p |
Dexamethasone better | Routine care better |
Effects of dexamethasone administration on 28-day mortality, by respiratory support method, obtained at randomization, and by the presence of any chronic disease3
| Dexamethasone | Routine care | RR (95% Cl) | |
| Lack of oxygen (x | 2 | = 0.08; p=0.78) | |
| 1 | |||
| Previous illness | 65/313 (20.8%) | 100/598 (16.7%) | 1.22 (0.89-1.66) |
Without prior disease | 24/188 (12.8%) | 45/436 (10.3%) | 1.12 (0.68-1.83) |
| Subtotal | 89/501 (17.8%) | 145/1034 (14.0%) | 1.19 (0.91-1.55) |
| Oxygen only (x | 2 | = 2.05; p=0.15 | |
| 1 | |||
| Previous illness | 221/702 (31.5%) | 481/1473 (32.7%) | 0.88 (0.75-1.03) |
Without prior disease | 77/577 (13.3%) | 201/1131 (17.8%) | 0.70 (0.54-0.91) |
| Subtotal | 298/1279 (23.3%) | 682/2604 (26.2%) | 0.82 (0.72-0.94) |
| Mechanical ventilation (x | 2 | = 1.52; p=0.22 | |
| 1 | |||
| Previous illness | 51/159 (32.1%) | 150/346 (43.4%) | 0.75 (0.54-1.02) |
Without prior disease | 44/165 (26.7%) | 133/337 (39.5%) | 0.56 (0.40-0.78) |
| Subtotal | 95/324 (29.3%) | 283/683 (41.4%) | 0.64 (0.51-0.81) |
| All participants | 482/2104(22.9%) | 1110/4321 (25.7%) | 0.83 (0.75-0.93) p |
Dexamethasone better | Routine care better |
1 www.recoverytrial.net
2, 3 (source: Horby P. et al., 2020; https://www.medrxiv.org/content/10.1101/2020.06.22.20137273v1;
doi: https://doi.org/10.1101/2020.06.22.20137273).
Pharmacokinetics
Dexamethasone binds to plasma albumin in a dose-dependent manner. At very high doses, most of it circulates freely in the blood. In hypoalbuminemia, the proportion of unbound (active) corticoid increases. In humans, after intravenous administration of radiolabeled dexamethasone, maximum levels of dexamethasone in the cerebrospinal fluid were observed 4 hours later, which were about 1/6 of the simultaneous concentration in plasma.
Dexamethasone, which has a biological half-life of more than 36 hours, is a glucocorticoid that retains its effectiveness for a very long time. Based on the long duration of action of dexamethasone, its daily continuous administration can at the same time lead to cumulation and overdose.
The half-life (serum time) of dexamethasone in adult patients is on average about 250 minutes (+ 80 minutes). Dexamethasone is excreted mainly by the kidneys, in the form of a free alcohol derivative. It is partially metabolized, the metabolites are excreted mainly by the kidneys in the form of glucuronates or sulfates. Impaired renal function does not significantly affect the excretion of dexamethasone. Severe liver disease prolongs the half-life.
Indication
Systemic application
- Brain swelling caused by brain tumor, neurosurgical interventions, brain abscess, bacterial meningitis.
- Polytraumatic shock/prevention of post-traumatic shock lung.
- Parenteral initial treatment of acute severe widespread skin diseases such as erythroderma, pemphigus vulgaris, acute eczema.
- Parenteral initial treatment of autoimmune diseases such as systemic lupus erythematosus (in particular the visceral form).
- Active rheumatoid arthritis with a severe progressive course, for example, forms accompanied by rapid destruction and/or extra-articular manifestations.
- Severe infectious diseases with toxic conditions (e.g. tuberculosis, typhus, brucellosis), only with simultaneous anti-infective therapy.
- Palliative therapy of malignant tumors.
- Prevention and treatment of postoperative or cytostatic-induced vomiting as part of antiemetic therapy regimens.
- Treatment of COVID-19 coronavirus disease in adults and adolescent patients (aged 12 years and over with a body weight of at least 40 kg) who require supplemental oxygen therapy.
Topical application
- Intra-articular injections: persistent inflammation in one or more joints after general treatment of chronic inflammatory joint diseases, synovitis in arthrosis, acute forms of shoulder-scapular periarthritis.
- Infiltration therapy (strictly according to indications): non-bacterial tendovaginitis and bursitis, periarthropathies, insertional tendopathies.
- Ophthalmology: subconjunctival use in non-infectious keratoconjunctivitis, scleritis (except necrotizing scleritis), anterior and intermediate uveitis.
Contraindication
Hypersensitivity to the active substance or to any of the excipients.
Intra-articular injection is contraindicated in:
- infections in the joint to be treated or in the immediate vicinity of it;
- bacterial arthritis;
- instability of the joint to be treated;
- bleeding tendency (spontaneous or associated with anticoagulant therapy);
- periarticular calcification;
- avascular necrosis of bone;
- severance of ties;
- Charcot joint.
Infiltration without appropriate additional therapy is prohibited for infections in the area of application, and subconjunctival use is also prohibited for eye diseases of a viral, bacterial or fungal nature, and for corneal injuries and ulcerative processes.
Interaction with other medicinal products and other types of interactions
Estrogens (e.g. ovulation inhibitors): The half-life of glucocorticoids may be prolonged, so their effects may be enhanced.
Drugs that induce CYP3A4, such as rifampicin, phenytoin, carbamazepine, barbiturates, and primidone: the effect of corticosteroids may be reduced.
CYP3A4 inhibitors (including ketoconazole, itraconazole, ritonavir, and cobicistat) may decrease the clearance of dexamethasone, leading to increased exposure and possible adrenal suppression/Cushing's syndrome. Such combinations should be avoided unless the potential benefit outweighs the increased risk of systemic corticosteroid side effects. In such cases, patients should be monitored for systemic corticosteroid effects.
Ephedrine: The metabolism of glucocorticoids may be accelerated and their effectiveness may be reduced.
Angiotensin-converting enzyme inhibitors: increased risk of changes in blood composition.
Cardiac glycosides: the effect of glycosides may be enhanced by potassium deficiency.
Saluretics/laxatives: increased potassium excretion is possible.
Antidiabetic agents: hypoglycemic efficacy may be reduced.
Coumarin derivatives: possible reduction or enhancement of anticoagulant effect. Concomitant use may require adjustment of anticoagulant dose.
Nonsteroidal anti-inflammatory drugs/antirheumatic drugs, salicylates and indomethacin: increased risk of gastrointestinal ulcers and bleeding.
Non-depolarizing muscle relaxants: longer duration of muscle relaxation is possible.
Atropine, other anticholinergics: with simultaneous use, an additional increase in intraocular pressure is possible.
Praziquantel: due to the use of corticosteroids, a decrease in the concentration of praziquantel in the blood is possible.
Chloroquine, hydroxychloroquine, mefloquine: there is an increased risk of myopathy, cardiomyopathy.
Protirelin: The effect of protirelin on increasing thyroid-stimulating hormone levels may be reduced.
Immunosuppressants: increased susceptibility to infection and possible worsening or manifestation of latent infections. Additionally for cyclosporine: cyclosporine blood levels increase, there is an increased risk of cerebral convulsions.
Fluoroquinolones may increase the risk of tendon-related disorders.
Impact on research methods: possible suppression of skin reactions during allergy diagnostics.
Application features
Treatment with dexamethasone sodium phosphate may lead to an increased risk of bacterial, viral, parasitic, fungal, and opportunistic infections due to immunosuppression. Symptoms of an existing or developing infection may be obscure, making diagnosis difficult. Reactivation of latent infections such as tuberculosis or hepatitis B may occur.
If a particularly stressful situation for the body occurs during therapy with Raft® (accident, surgery, childbirth, etc.), a temporary dose increase may be necessary.
Therapy with Raft® should only be carried out in strict accordance with the indications and, if necessary, accompanied by additional targeted anti-infective therapy for the following diseases:
- acute viral infections (hepatitis B, shingles, Herpes simplex, chickenpox, herpetic keratitis);
- HBsAg-positive chronic active hepatitis;
- about 8 weeks before and up to 2 weeks after preventive vaccinations using live vaccines;
- systemic mycoses and parasitic diseases (e.g. nematodoses);
- in patients with suspected or confirmed strongyloidiasis (an infection caused by intestinal hookworm), glucocorticoids may lead to activation and massive multiplication of parasites;
- poliomyelitis;
- lymphadenitis after BCG vaccination;
- acute and chronic bacterial infections;
- if there is a history of tuberculosis - use only under the protection of tuberculostatic agents.
In addition, therapy with the drug Raft® should be carried out strictly according to indications, and, if necessary, be accompanied by additional special therapy, in the presence of:
- gastrointestinal ulcer disease;
- osteoporosis;
- severe heart failure;
- difficultly controlled hypertension;
- difficultly controlled diabetes;
- psychiatric diseases (including history), including suicidal thoughts: neurological or psychiatric monitoring is recommended;
- for narrow-angle and open-angle glaucoma: ophthalmological monitoring and supportive therapy are recommended;
- trophic changes of the cornea and corneal injuries: ophthalmological monitoring and supportive therapy are recommended.
Vision impairment
Visual disturbances may occur with systemic and topical corticosteroids. If a patient experiences symptoms such as blurred vision or other visual disturbances, an ophthalmologist should be consulted to evaluate possible causes. Causes may include cataracts, glaucoma, or rare conditions such as central serous chorioretinopathy (CSC), which have been reported following systemic or topical corticosteroid use.
Due to the risk of intestinal perforation, Raft® should only be used if there are justified indications and under appropriate monitoring in:
- severe ulcerative colitis with the threat of perforation, possibly without peritoneal irritation;
- diverticulitis;
- enteroanastomosis (immediately postoperative).
Patients receiving high doses of glucocorticoids may not show signs of peritoneal irritation after gastrointestinal perforation.
When using Raft® for diabetics, it is necessary to take into account the possible increase in the need for insulin or oral antidiabetic agents.
Regular monitoring of blood pressure is required when using Raft®, particularly when using high doses and in patients with poorly controlled hypertension.
Close monitoring is necessary for patients with severe heart failure, as there is a risk of worsening of the condition.
Bradycardia may occur when taking high doses of dexamethasone.
Serious anaphylactic reactions are possible.
There is an increased risk of tendon disorders, tendinitis and tendon ruptures when fluoroquinolones and glucocorticoids are taken simultaneously.
Possible worsening of concomitant myasthenia gravis at the beginning of treatment with Raft®.
Vaccinations using killed vaccines are possible. However, when using high doses of corticosteroids, it is necessary to consider the possible deterioration of the immune response and the impact on the success of vaccinations.
At high doses, serum potassium levels should be monitored, attention should be paid to adequate potassium intake and sodium restriction.
Abrupt discontinuation of therapy for more than 10 days may lead to exacerbation or relapse of the underlying disease, as well as the development of acute adrenal insufficiency/cortisone withdrawal syndrome; therefore, when therapy is expected to be discontinued, the dose should be reduced slowly.
In post-marketing surveillance of patients with hematological malignancies, tumor lysis syndrome (TLS) has been observed after the use of dexamethasone or dexamethasone in combination with other chemotherapeutic agents. Patients at increased risk of tumor lysis syndrome (TLS), such as those with a high degree of proliferation, high tumor burden and high sensitivity to cytostatics, should be closely monitored and treated with appropriate precautions.
Intravenous injections should be performed slowly (over 2–3 minutes), as too rapid an injection lasting less than 3 minutes may result in harmless side effects in the form of "creeping goosebumps" or paresthesia.
Raft® is a short-term medication. When used without appropriate instructions for a long period of time, all warnings and precautions used with long-term use of glucocorticoid-containing medications should be observed.
When used topically, attention should be paid to possible systemic side effects and interactions.
Intra-articular use of glucocorticoids increases the risk of infectious diseases of the joints.
Prolonged and repeated use of glucocorticoids in weight-bearing joints may worsen wear-and-tear changes in the joints. This may be due to overloading the joint after pain or other symptoms have subsided.
Topical use in ophthalmology.
Cushing's syndrome and/or adrenal suppression may occur after intensive or prolonged treatment due to systemic absorption of ophthalmic dexamethasone in susceptible patients, including children and patients treated with CYP3A4 inhibitors (including ritonavir and cobicistat). In such cases, treatment should be discontinued gradually.
Elderly patients.
Since elderly patients are at increased risk of osteoporosis, the benefit-risk ratio of Raft® therapy should be carefully weighed.
The use of Raft® may lead to positive results in doping tests.
Raft® contains less than 1 mmol (23 mg) sodium per dose, i.e. essentially sodium-free.
Use during pregnancy or breastfeeding
Pregnancy.
Dexamethasone crosses the placenta.
During pregnancy, especially during the first 3 months, use should only occur after careful assessment of the benefit-risk ratio.
Long-term therapy with glucocorticoids during pregnancy may cause fetal developmental disorders.
Animal studies have shown that corticosteroids can cause fetal malformations, including cleft palate, intrauterine growth retardation, and effects on brain growth and development. There is no evidence that corticosteroids increase the incidence of congenital anomalies such as cleft palate/cleft lip in humans.
When taking glucocorticoids at the end of pregnancy, there is a risk of atrophy of the adrenal cortex in the fetus, which may require replacement therapy in the newborn.
Breastfeeding period.
Dexamethasone passes into breast milk. It is not yet known whether it is harmful to the infant. However, its use during breastfeeding should be carefully justified. If increased doses are required for medical reasons, breastfeeding should be discontinued.
Ability to influence reaction speed when driving vehicles or other mechanisms
There are still no indications that the use of Raft® impairs the ability to drive or operate other mechanisms.
Method of administration and doses
Dosage.
The dosage depends on the type and severity of the disease, as well as the individual patient's response to therapy. Relatively high initial doses are generally used, which should be significantly higher in acute diseases with a severe course than in chronic diseases.
Unless otherwise recommended, the following scheme should be used.
Systemic application:
- cerebral edema: depending on the cause and severity, the initial dose is 8–10 mg (up to 80 mg) intravenously (IV), then 16–24 mg (up to 48 mg) per day divided into 3–4 (6) single IV doses for 4–8 days. During radiation therapy, as well as during conservative therapy of inoperable brain tumors, a longer-term need for lower doses of dexamethasone may arise.
- Brain swelling due to bacterial meningitis: 0.15 mg/kg body weight every 6 hours for 4 days, for children – 0.4 mg/kg body weight every 12 hours for 2 days; starting before the first dose of antibiotics.
- Post-traumatic shock/prevention of post-traumatic shock lung: initial dose 40–100 mg (children 40 mg) IV, repeat dose after 12 hours or every 6 hours 16–40 mg for 2–3 days.
- Acute severe asthma attack. Adults: emergency injection of 8–20 mg IV, if necessary repeated injections of 8 mg every 4 hours. Children: 0.15–0.3 mg/kg body weight IV or orally in an appropriate form, or 1.2 mg/kg body weight bolus, then 0.3 mg/kg body weight every 4–6 hours. Aminophylline and secretolytic agents can be used additionally.
- Acute forms of skin diseases: depending on the type and severity of the disease, daily doses are 8–40 mg intravenously, in some cases up to 100 mg. Further treatment is by switching to oral forms with a gradual decrease in dosage.
- Active phases of rheumatic systemic diseases: systemic lupus erythematosus 6–16 mg/day.
- Active rheumatoid arthritis with severe progressive course: in forms accompanied by rapid destruction: 12–16 mg/day, in extra-articular manifestations: 6–12 mg/day.
- Severe infectious diseases, toxic conditions (e.g. tuberculosis, typhoid fever; only with simultaneous appropriate anti-infective therapy) 4–20 mg/day intravenously, in some cases (e.g. typhoid fever) the initial dose may be up to 200 mg.
- Palliative therapy of malignant tumors: initially 8–16 mg/day, with continued long-term therapy 4–12 mg/day.
- Prevention and treatment of cytostatic therapy-induced vomiting as part of antiemetic therapy regimens: 10–20 mg IV or orally in an appropriate form before the start of chemotherapy, then, if necessary, 4–8 mg 2 to 3 times daily for 1–3 days (with moderately emetogenic chemotherapy) or up to 6 days (highly emetogenic chemotherapy).
- Prevention and treatment of postoperative vomiting: a single dose of 8–20 mg IV before the start of surgery, for children aged 2 years and older: 0.15–0.5 mg/kg body weight (maximum 16 mg).
- Treatment of coronavirus disease COVID-19:
Adults and children (adolescents aged 12 years and older with a body weight of at least 40 kg): 6 mg of dexamethasone intravenously once a day for up to 10 days.
Topical application
Local infiltration and injection therapy should be performed in most cases by using 4–8 mg; for injection into small joints and subconjunctival administration, 2 mg of dexamethasone phosphate is sufficient.
Method of administration and doses
When intravenous injections or infusions, the drug should be administered slowly (2–3 minutes); if intravenous injection is not possible and hemodynamics are intact, intramuscular injections are possible. In addition, Raft® can be used by infiltration, intraarticularly or subconjunctivally. The duration of use is determined according to the indications.
In hypothyroidism or cirrhosis of the liver, relatively low dosages may be sufficient or a dose reduction may be required.
Intra-articular injections are considered open interventions and should only be performed under strictly aseptic conditions. As a rule, a single intra-articular injection is sufficient to successfully alleviate the symptom. If a repeat injection is necessary, such an injection should be performed no earlier than after 3-4 weeks. The number of injections per joint is limited and should not exceed 3-4 injections. After a repeat injection, the condition of the joint must be monitored by a doctor.
Infiltration: Infiltration is performed in the area of greatest pain or at the tendon insertion site. Intratendinous injections are not permitted! Injections should be avoided at close distances from each other. Care should be taken to observe strict aseptic precautions.
Suitability of the solution.
Only clear solutions may be used. The contents of the ampoule are for single use only. Any remaining solution for injection should be discarded.
The drug is compatible with the following infusion solutions (250 and 500 ml, respectively) and can be used within 24 hours:
- isotonic saline solution;
- Ringer's solution;
- 5% glucose solution.
When combining with other infusion solutions, attention should be paid to the information of the relevant suppliers, taking into account compatibilities, contraindications, side effects and interactions.
Children.
When used early (less than 96 hours after birth) in premature infants with chronic lung disease, starting doses of 0.25 mg/kg twice daily have been shown to have negative long-term effects on neurodevelopment.
When deciding on Raft® therapy for children in the growth phase, the benefit-risk ratio should be carefully analyzed.
Overdose
Acute dexamethasone poisoning is unknown. In chronic overdose, adverse reactions are increased, especially from the endocrine system, metabolism and electrolyte balance.
Adverse reactions
With short-term dexamethasone therapy, the risk of adverse reactions is insignificant, the exception is parenteral therapy using high doses, in which attention should be paid to electrolyte imbalance, edema formation, possible increase in blood pressure, heart failure, heart rhythm disturbances or seizures, and, including with short-term use, clinical manifestations of infections are possible.
The following side effects are possible, they largely depend on the dose and duration of therapy, therefore the frequency of occurrence of such side effects cannot be specified:
Infections and parasitic diseases: masking of infections, manifestations, exacerbation or reactivation of viral infections, fungal infections, bacterial, parasitic infections, as well as infections caused by opportunistic microorganisms, activation of strongyloidiasis.
From the blood and lymphatic system: moderate leukocytosis, lymphopenia, eosinopenia, polycythemia.
Immune system: hypersensitivity reactions (e.g. drug rash), serious anaphylactic reactions such as arrhythmia, bronchospasm, hypotension or hypertension, vascular collapse, cardiac arrest, weakened immune defense.
Endocrine diseases: Cushing's syndrome (typical symptoms: moon-shaped face, obesity of the trunk and plethora (fullness of blood)), adrenal suppression.
Metabolism and digestion: sodium retention with edema formation, increased potassium excretion (caution: arrhythmia), weight gain, decreased glucose tolerance, diabetes mellitus, hypercholesterolemia and hypertriglyceridemia, increased appetite.
Psychiatric diseases: depression, irritability, euphoria, mood swings, psychosis, mania, hallucinations, affective lability, feelings of fear, sleep disturbances, suicidal tendencies.
From the nervous system: cerebellar pseudotumor, manifestation of latent epilepsy, increased readiness for attack in manifest epilepsy.
On the part of the organs of vision: cataract, in particular with posterior subcapsular opacification, glaucoma, worsening of symptoms in corneal ulcers, susceptibility to viral, fungal and bacterial eye inflammations, exacerbation of bacterial inflammations in the cornea of the eye, ptosis of the upper eyelid, dilated pupils, chemosis, iatrogenic scleral perforation, chorioretinopathy. In some cases - reversible exophthalmos, with subconjunctival use - herpetic keratitis, corneal perforation in existing keratitis, blurred vision.
On the part of blood vessels: hypertension, increased risk of arteriosclerosis and thrombosis, vasculitis (as well as withdrawal syndrome after long-term therapy), increased capillary fragility.
Gastrointestinal: stomach and intestinal ulcers, gastrointestinal bleeding, pancreatitis, stomach pain.
Skin and subcutaneous tissue disorders: striae, atrophy, telangiectasia, petechiae, ecchymoses, hypertrichosis, steroid acne, rosacea-like (perioral) dermatitis, changes in skin pigmentation.
On the part of skeletal muscles, connective tissue and bones: myopathy, muscle atrophy and muscle weakness, osteoporosis (depending on the dose, also possible with short-term use), aseptic bone necrosis, tendon diseases, tendinitis, ligament rupture, epidural lipomatosis, growth retardation in children.
Diseases of the genitals and mammary glands: impaired secretion of sex hormones (resulting in the occurrence of such phenomena as irregular menstruation, amenorrhea, hirsutism, impotence).
General disorders and local manifestations: delayed wound healing.
Topical use: local irritation and symptoms of incompatibility (feeling of heat, prolonged pain) are possible, especially when used in the eyes. If care is not taken when injecting a corticosteroid into the joint cavity, the development of skin atrophy and subcutaneous tissue atrophy at the injection site cannot be ruled out.
Expiration date
2 years.
Do not use the drug after the expiration date indicated on the package.
Storage conditions
Store in
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.







