Risperidone oral solution with dispenser 1 mg/ml bottle 30 ml
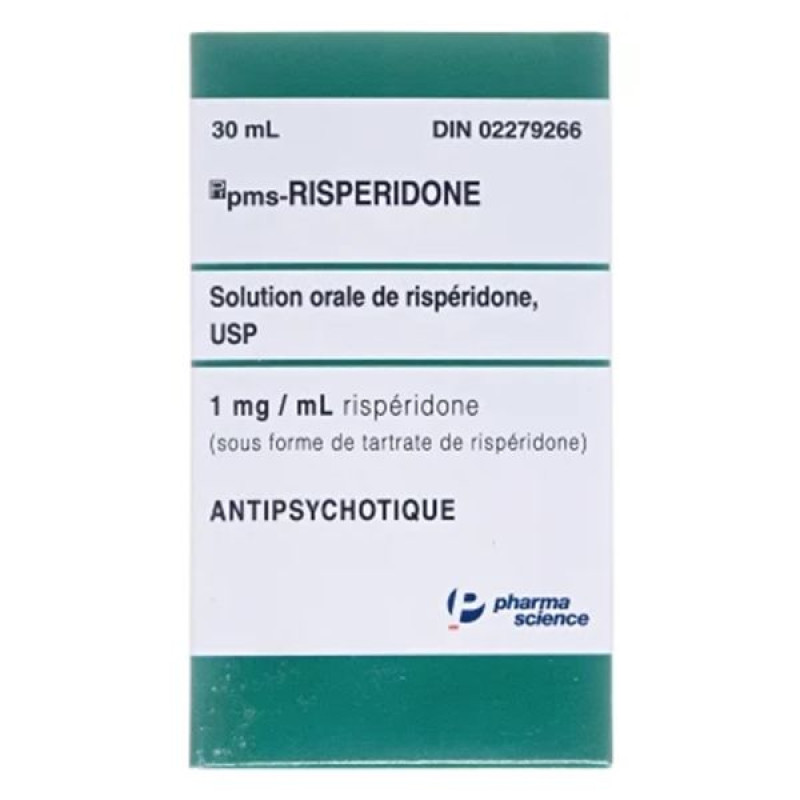
Instructions Risperdal oral solution with dispenser 1 mg/ml bottle 30 ml
Composition
active ingredient: risperidone;
1 ml of solution contains 1 mg of risperidone;
excipients: purified water, benzoic acid (E 210), tartaric acid, sodium hydroxide, sorbitol solution (E 420).
Dosage form
Oral solution.
Main physicochemical properties: clear, odorless liquid.
Pharmacotherapeutic group
Antipsychotics. ATX code N05A X08.
Pharmacological properties
Pharmacodynamics.
Risperidone is a selective monoaminergic antagonist with unique properties. It exhibits high affinity for serotonergic 5-HT2 and dopaminergic D2 receptors. Risperidone also binds to α1-adrenergic receptors and, with lower affinity, to H1-histaminergic and α2-adrenergic receptors. Risperidone has no affinity for cholinergic receptors. Although risperidone is a potent D2 antagonist, which is associated with its efficacy in the productive symptoms of schizophrenia, it does not cause significant motor depression and induces catalepsy to a lesser extent than classical neuroleptics. Balanced central antagonism towards serotonin and dopamine reduces the tendency towards extrapyramidal side effects and extends the therapeutic effect of the drug to cover the negative and affective symptoms of schizophrenia.
Pharmacokinetics.
Risperidone is metabolized to 9-hydroxyrisperidone, which has similar pharmacological effects to risperidone.
Absorption. After oral administration, risperidone is completely absorbed and reaches peak plasma concentrations within 1–2 hours, in elderly patients within 2–3 hours. The absolute bioavailability after oral administration of risperidone is 70% (CV = 25%). Food does not affect the absorption of the drug, so risperidone can be taken regardless of meals. The absolute bioavailability is 66% in extensive metabolizers and 82% in poor metabolizers.
Distribution. Risperidone is rapidly distributed in the body. The volume of distribution is 1–2 l/kg. In plasma, risperidone binds to albumin and α1-acid glycoprotein. Risperidone is 90% bound to plasma proteins, 9-hydroxyrisperidone is 77%. Steady-state concentrations of risperidone are reached in most patients within 1 day. Steady-state concentrations of 9-hydroxyrisperidone are reached within 4–5 days.
Biotransformation and elimination. Risperidone is metabolized by cytochrome CYP2D6 to 9-hydroxyrisperidone, which has similar pharmacological effects to risperidone. Risperidone and 9-hydroxyrisperidone form the active antipsychotic fraction. Cytochrome CYP2D6 is subject to genetic polymorphism. In extensive CYP2D6 metabolizers, risperidone is rapidly converted to 9-hydroxyrisperidone, whereas in poor metabolizers, risperidone is converted much more slowly. Although extensive metabolizers have lower concentrations of risperidone and 9-hydroxyrisperidone than in poor metabolizers, the pharmacokinetics of risperidone and 9-hydroxyrisperidone in combination (i.e., the active antipsychotic fraction) after single and multiple doses are similar in extensive and poor metabolizers of CYP2D6.
Another route of metabolism of risperidone is N-dealkylation. In vitro studies with human liver microsomes have shown that risperidone at clinically relevant concentrations does not significantly inhibit the metabolism of drugs metabolized by cytochrome P450 isoenzymes, including CYP1A2, CYP2A6, CYP2C8/9/10, CYP2D6, CYP2E1, CYP3A4, and CYP3A5. One week after administration, 70% of the dose is excreted in the urine and 14% in the feces. The concentration of risperidone and 9-hydroxyrisperidone in the urine is 35–45% of the dose taken. The rest is made up of inactive metabolites. After oral administration in psychotic patients, the half-life is approximately 3 hours. The half-life of 9-hydroxyrisperidone and the active antipsychotic fraction reaches 24 hours, and in elderly patients - 34 hours.
Linearity: Plasma concentrations of risperidone are proportional to the dose of the drug (within the therapeutic dose range).
Elderly patients and patients with impaired renal or hepatic function. A pharmacokinetic study of a single dose of the drug in elderly patients demonstrated that such patients had a 43% higher concentration of the active antipsychotic fraction, a 38% longer half-life, and a 30% reduced clearance of the active antipsychotic fraction.
After oral administration, the clearance and half-life of risperidone and the active antipsychotic fraction in patients with moderate and severe hepatic impairment were not significantly different from those in young healthy volunteers.
Children: The pharmacokinetics of risperidone, 9-hydroxyrisperidone and the active antipsychotic fraction in children are similar to those in adults.
Gender, race, and smoking: A population pharmacokinetic analysis revealed no apparent effect of gender, age, or smoking status on the pharmacokinetics of risperidone or the active antipsychotic fraction.
Indication
For the treatment of schizophrenia;
for the treatment of moderate to severe manic episodes in bipolar disorder;
for the short-term treatment (up to 6 weeks) of severe aggression in patients with moderate to severe Alzheimer's dementia who are at risk of harm to themselves or others and who have not responded to non-pharmacological treatments (see sections "Method of administration and dosage" and "Special instructions for use");
for the symptomatic short-term treatment (up to 6 weeks) of severe aggression in conduct disorders in children from 5 years of age and adolescents with below average mental development or mental retardation diagnosed according to DSM-IV criteria, in whom the severity of aggressive or other destructive behavior requires pharmacological treatment. Pharmacological treatment should be an integral part of a comprehensive treatment program that includes psychological support and educational measures. It is recommended that Risperidone be prescribed by a specialist in the field of child neurology, child and adolescent psychiatry or a physician experienced in the treatment of conduct disorders in children and adolescents.
Contraindication
Hypersensitivity to the active ingredient or to any excipient of the medicinal product.
Dementia and symptoms of Parkinson's disease (rigidity, bradykinesia and parkinsonian postural disorders).
Dementia and suspected dementia with Lewy bodies (in addition to symptoms of dementia, at least two of the following symptoms: parkinsonism, visual hallucinations, unsteadiness of gait).
Interaction with other medicinal products and other types of interactions
Pharmacodynamic interactions.
Drugs that prolong the QT interval.
Caution should be exercised when prescribing antipsychotics, including risperidone, with drugs that prolong the QT interval, such as antiarrhythmics (quinidine, disopyramide, procainamide, propafenone, amiodarone, sotalol), tricyclic antidepressants (amitriptyline), tetracyclic antidepressants (maprolitine), some antihistamines, other antipsychotics, some antimalarials (quinine, mefloquine), drugs that cause electrolyte imbalance (hypokalemia, hypomagnesemia), bradycardia, and drugs that inhibit the hepatic metabolism of risperidone. This list is indicative and not exhaustive.
Centrally acting drugs and alcohol.
Risperidone should be used with caution in combination with other centrally acting substances, including alcohol, opiates, antihistamines and benzodiazepines, due to an increased risk of sedation.
Levodopa and dopamine agonists.
Risperidone may have antagonistic effects on levodopa and other dopamine antagonists. If such a combination is considered essential, particularly in end-stage Parkinson's disease, the lowest effective doses of each drug should be used.
Medicines with hypotensive effect.
In the post-marketing period, cases of clinically significant hypotension have been observed with the concomitant use of risperidone and antihypertensive drugs.
Psychostimulants.
The use of risperidone in combination with psychostimulants (e.g. methylphenidate) may cause the appearance of extrapyramidal symptoms after dose adjustment of one or both drugs (see section "Special warnings and precautions for use").
Paliperidone.
Concomitant use of oral Risperidone with paliperidone is not recommended, as paliperidone is the active metabolite of risperidone and their combination may lead to additive effects of the active antipsychotic fraction.
Pharmacokinetic interactions.
Food does not affect the absorption of Risperidone.
Risperidone is primarily metabolized by CYP2D6 and to a lesser extent by CYP3A4. Risperidone and its active metabolite 9-hydroxyrisperidone are substrates of P-glycoprotein (P-gp). Substances that modify CYP2D6 activity, as well as potent inhibitors or inducers of CYP3A4 and/or P-gp activity, may affect the pharmacokinetics of the active antipsychotic fraction of risperidone.
Potent CYP2D6 inhibitors.
CYP3A4 and P-gp inhibitors.
Concomitant use of Risperidone with potent CYP3A4 and/or P-gp inhibitors may significantly increase the plasma concentration of the active antipsychotic fraction of risperidone. At the beginning of concomitant use, as well as in the event of discontinuation of itraconazole or other potent CYP3A4 and/or P-glycoprotein inhibitors, the physician should review the dose of Risperidone.
CYP3A4 and P-gp inducers.
Concomitant use of Risperidone with strong CYP3A4 and/or P-gp inducers may reduce the plasma concentration of the active antipsychotic fraction of risperidone. At the beginning of therapy, as well as in the event of discontinuation of carbamazepine or other strong CYP3A4/P-glycoprotein inducers, the physician should review the dose of Risperidone. The effect of CYP3A4 inducers is time-dependent: the maximum effect may be achieved at least 2 weeks after the start of treatment. Accordingly, CYP3A4 induction may persist for at least 2 weeks after discontinuation.
Drugs with a high degree of protein binding.
When risperidone was used with other drugs that are extensively bound to plasma proteins, no clinically significant displacement of either drug from the protein fraction was observed. In case of concomitant use with such a drug, the product information for the drug should be consulted regarding metabolic pathways and the need for dose adjustment.
Children.
Interaction studies have only been conducted in adult patients. It is not known whether the results can be applied to children.
Concomitant use of psychostimulants (e.g. methylphenidate) with Risperidone in children did not affect the pharmacokinetics and efficacy of Risperidone.
Effect of other drugs on the pharmacokinetics of risperidone.
Antibacterial drugs
Erythromycin, a moderate CYP3A4 inhibitor and P-gp inhibitor, does not alter the pharmacokinetics of risperidone and the active antipsychotic fraction.
Rifampicin, a potent CYP3A4 inducer and P-gp inducer, reduces the concentration of the active antipsychotic fraction in blood plasma.
Cholinesterase inhibitors
Donepezil and galantamine, substrates of CYP2D6 and CYP3A4, do not demonstrate a clinically significant effect on the pharmacokinetics of risperidone and the active antipsychotic fraction.
Antiepileptic drugs
Carbamazepine, a potent CYP3A4 and P-gp inducer, decreased plasma concentrations of the active antipsychotic fraction of risperidone. A similar effect may be observed with phenytoin and phenobarbital, which are also inducers of the hepatic enzymes CYP3A4 and P-glycoprotein.
Topiramate modestly reduces the bioavailability of risperidone and does not affect the bioavailability of the active antipsychotic fraction. This interaction is unlikely to have a clinically significant effect.
Antifungal medications
Itraconazole, a potent CYP3A4 inhibitor and P-gp inhibitor, at a dose of 200 mg per day increases the concentration of the active antipsychotic fraction in blood plasma by approximately 70% when co-administered with risperidone at doses of 2 to 8 mg per day.
Ketoconazole, a potent CYP3A4 inhibitor and P-gp inhibitor, at a dose of 200 mg per day increases the concentration of risperidone and reduces the concentration of 9-hydroxyrisperidone in blood plasma.
Antipsychotic medications
Phenothiazines may increase the plasma concentration of risperidone, but not the active antipsychotic fraction.
Antiviral drugs
Protease inhibitors: no data available; since ritonavir is a potent CYP3A4 inhibitor and a weak CYP2D6 inhibitor, ritonavir and ritonavir-boosted protease inhibitors may increase the concentration of the active antipsychotic fraction of risperidone.
Beta-blockers
Some beta-blockers may increase the concentration of risperidone, but do not affect the concentration of the active antipsychotic fraction in the blood plasma.
Calcium channel blockers
Verapamil, a moderate CYP3A4 inhibitor and P-gp inhibitor, increases the plasma concentrations of risperidone and the active antipsychotic fraction.
Medicines for the treatment of gastrointestinal diseases
H2-receptor antagonists: cimetidine and ranitidine, weak inhibitors of CYP2D6 and CYP3A4, increase the bioavailability of risperidone and minimally affect the bioavailability of the active antipsychotic fraction.
SSRIs [selective serotonin reuptake inhibitors] and tricyclic antidepressants
Fluoxetine, a potent CYP2D6 inhibitor, increases the plasma concentration of risperidone, but less than the concentration of the active antipsychotic fraction.
Paroxetine, a potent CYP2D6 inhibitor, increases risperidone plasma concentrations, but (up to 20 mg/day) to a lesser extent than the concentration of the active antipsychotic fraction. However, higher doses of paroxetine may increase the concentration of the active antipsychotic fraction.
Sertraline, a weak CYP2D6 inhibitor, and fluvoxamine, a weak CYP3A4 inhibitor, at doses up to 100 mg/day do not cause clinically important changes in the concentration of the active antipsychotic fraction of risperidone. However, doses of sertraline or fluvoxamine exceeding 100 mg/day may increase the concentration of the active antipsychotic fraction of risperidone.
The effect of risperidone on the pharmacokinetics of other drugs.
Antiepileptic drugs
Risperidone has no clinically important effect on the pharmacokinetics of valproate or topiramate.
Antipsychotic medications
Aripiprazole, a CYP2D6 and CYP3A4 substrate: oral or injectable risperidone formulations do not affect the pharmacokinetics of aripiprazole and its active metabolite dehydroaripiprazole.
Digitalis glycosides
Risperidone has no clinically significant effect on the pharmacokinetics of digoxin.
Lithium
Risperidone has no clinically important effect on the pharmacokinetics of lithium.
Concomitant use of risperidone with furosemide.
See section "Special warnings and precautions for use" regarding increased mortality in elderly patients with dementia when used concomitantly with furosemide.
Application features
Elderly patients with dementia.
Increased mortality rate.
Elderly patients with dementia treated with atypical antipsychotics had an increased mortality rate compared with placebo, according to a meta-analysis of 17 controlled trials of atypical antipsychotics, including risperidone. In a placebo-controlled trial of risperidone, the mortality rate in this group was 4.0% compared with 3.1% in the placebo group. The diagnostic odds ratio (95% confidence interval) was 1.21 (0.7, 2.1). The median age of patients who died was 86 years (range, 67–100 years).
Evidence from two large observational studies suggests that older people with dementia who were treated with conventional (typical) antipsychotics had a slightly increased risk of death compared with patients who were not treated with antipsychotics. The exact level of this risk cannot be determined from the available study data, and the reason for the increased risk is unknown.
Concomitant use with furosemide: In a placebo-controlled study in elderly patients with dementia, an increased mortality rate was observed with the concomitant use of risperidone with furosemide (7.3%; mean age 89 years, range 75–97 years) compared with patients treated with risperidone alone (3.1%; mean age 84 years, range 70–96 years) or furosemide alone (4.1%; mean age 80 years, range 67–90 years). An increased mortality rate among patients treated with risperidone and furosemide concomitantly was observed in two of the four clinical trials. No increased mortality rate was observed in patients treated with risperidone concomitantly with other diuretics.
No pathophysiological mechanisms have been identified to explain this finding. The cause of death was not uniform. However, caution should be exercised when prescribing the drug in such cases, and the risks and benefits of this combination or of other potential diuretics should be assessed before prescribing the drug. No increased mortality was observed in patients taking other diuretics with risperidone. Regardless of treatment, dehydration was a common risk factor for death and should be carefully monitored in patients with dementia.
Cerebrovascular adverse reactions (CVAR).
In placebo-controlled clinical trials, patients with dementia treated with risperidone had a higher rate (approximately 3-fold) of fatal cerebrovascular adverse events (strokes and transient ischemic attacks) compared with those treated with placebo (mean age 85 years; range 73–97 years).
Pooled data from six placebo-controlled trials in elderly patients with dementia (aged 65 years and older) showed that cerebrovascular events (serious and non-serious, combined) occurred in 3.3% (33/1009) of risperidone-treated patients compared with 1.2% (8/712) of placebo-treated patients. The risperidone-to-placebo ratio (odds ratio; 95% CI) was 2.96 (1.34, 7.50). The mechanism of this increased risk is unknown. An increased risk of CVD cannot be excluded with other antipsychotics or in other patient populations. Risperidone should be used with caution in patients with risk factors for stroke.
The risks and benefits of prescribing Risperidone to elderly patients with dementia should be carefully weighed, especially the risk of stroke. Patients and caregivers should be instructed to report promptly any signs of possible cerebrovascular events, such as sudden weakness, numbness of the face, arms or legs, or speech or vision problems. In such cases, all possible treatment options, including discontinuation of risperidone, should be considered immediately.
For persistent aggression in patients with moderate to severe Alzheimer's disease, Risperidone is prescribed only for short-term use as an adjunct to non-pharmacological measures that have shown limited or no efficacy, provided that there is no potential threat of harm to self or others.
During treatment, patients should be regularly assessed and the need for further therapy reviewed.
Orthostatic hypotension.
Due to the α1-lytic activity of risperidone, orthostatic hypotension may occur, especially at the beginning of treatment. In the post-marketing period, clinically significant hypotension has been observed with the concomitant use of risperidone and antihypertensive agents. Risperidone should be used with caution in patients with cardiovascular disease (such as heart failure, myocardial infarction, conduction disorders, dehydration, hypovolemia or cerebrovascular disease). In these cases, the dose should be adjusted gradually (see section "Method of administration and dosage"). If hypotension occurs, a dose reduction should be considered.
Leukopenia, neutropenia, agranulocytosis.
Leukopenia, neutropenia and agranulocytosis have been reported with antipsychotics, including risperidone. Agranulocytosis has been reported very rarely (< 1/10,000 patients) in the post-marketing setting.
Patients with a history of significant leukopenia or drug-induced leukopenia/neutropenia should be closely monitored during the first few months of treatment and risperidone should be discontinued if there is evidence of significant leukopenia in the absence of other causes for the decrease.
Patients with clinically significant neutropenia should be monitored for fever and other signs of infection and treated appropriately if symptoms develop. In case of severe neutropenia (< 1 × 109/l), risperidone treatment should be discontinued and the white blood cell count monitored until recovery.
Tardive dyskinesia/extrapyramidal symptoms.
Tardive dyskinesia, characterized by involuntary rhythmic movements (predominantly of the tongue and/or face), has been reported with dopamine receptor antagonists. The occurrence of extrapyramidal symptoms is a risk factor for the development of tardive dyskinesia. If signs and symptoms of tardive dyskinesia develop, discontinuation of all antipsychotic medications should be considered.
Caution should be exercised when psychostimulants (e.g. methylphenidate) and risperidone are used concomitantly, as extrapyramidal symptoms may occur when adjusting the dose of either drug. Gradual withdrawal of psychostimulant treatment is recommended (see section 4.5).
Neuroleptic malignant syndrome.
Rare cases of neuroleptic malignant syndrome, characterized by hyperthermia, muscle rigidity, autonomic instability, impaired consciousness, and elevated creatine phosphokinase levels, have been reported with classical neuroleptic drugs. Additional features include myoglobinuria (rhabdomyolysis) and acute renal failure. If neuroleptic malignant syndrome develops, all antipsychotic drugs, including Risperidone, should be discontinued.
Parkinson's disease and dementia with Lewy bodies.
Physicians should weigh the risks of using antipsychotics, including RISPERDAL, in patients with Parkinson's disease or dementia with Lewy bodies (see Contraindications). Risperidone may worsen Parkinson's disease. Patients with any of the above conditions may be at increased risk of neuroleptic malignant syndrome and may be more sensitive to antipsychotics (e.g., confusion, pain sensitivity, and postural instability with frequent falls in addition to extrapyramidal symptoms).
Hyperglycemia, diabetes mellitus, and exacerbation of pre-existing diabetes mellitus have been reported with risperidone. In some cases, patients had a pre-existing overweight status, which may have been a predisposing factor. Ketoacidosis and, rarely, diabetic coma have been reported. Appropriate clinical monitoring is recommended in accordance with the guidelines for the use of antipsychotics. Patients taking any atypical antipsychotic, including RISPERDAL, should be observed for symptoms of hyperglycemia (such as polydipsia, polyuria, polyphagia, and weakness), and patients with diabetes mellitus should be monitored regularly for worsening of glucose control.
Weight gain.
Significant weight gain has been reported with risperidone. Weight monitoring is recommended.
Hyperprolactinemia.
Hyperprolactinemia is a common adverse event during treatment with risperidone. Monitoring of prolactin levels is recommended in patients who experience adverse events that may be related to plasma prolactin levels (e.g. gynecomastia, menstrual disorders, anovulation, impaired fertility, decreased libido, erectile dysfunction and galactorrhea).
Tissue culture studies suggest that cell growth in human breast tumors may be stimulated by prolactin. Although a clear association with antipsychotic use has not yet been established in clinical or epidemiological studies, caution is advised when prescribing risperidone to patients with a history of such conditions. Risperidone should be used with caution in patients with hyperprolactinemia and in patients with prolactin-dependent tumors.
QT prolongation.
In the post-marketing period, QT prolongation has been observed very rarely. As with other antipsychotics, risperidone should be used with caution in patients with cardiovascular disease, a family history of QT prolongation, bradycardia, or electrolyte disturbances (hypokalemia, hypomagnesemia), as this increases the risk of arrhythmogenic effects. Caution is also required when risperidone is used concomitantly with other drugs that prolong the QT interval.
Convulsions
Risperidone should be used with caution in patients with a history of seizures or other conditions that potentially lower the seizure threshold.
Priapism.
There is a possibility of priapism during treatment with risperidone due to its alpha-adrenergic blocking effect.
Body temperature regulation.
Antipsychotic drugs may impair the body's ability to lower core body temperature. Appropriate care is recommended for patients prescribed risperidone in conditions where core body temperature may increase, such as: intense physical exercise, exposure to high ambient temperatures, concomitant therapy with drugs with anticholinergic activity, or exposure to dehydration.
Antiemetic effect.
In preclinical studies, risperidone has been shown to have an antiemetic effect. This property may mask the symptoms of overdose with certain drugs or conditions such as intestinal obstruction, Reye's syndrome, and brain tumors.
Liver and kidney dysfunction.
Patients with impaired renal function have a reduced ability to excrete the active antipsychotic fraction of the drug compared to patients with normal renal function. In patients with impaired hepatic function, an increase in the concentration of the free fraction of risperidone in the blood plasma is observed (see section "Method of administration and dosage").
Venous thromboembolism.
Cases of venous thromboembolism have been described with the use of antipsychotic drugs. Since patients treated with antipsychotic drugs often have acquired risk factors for venous thromboembolism, all possible risk factors for the development of thromboembolism should be identified before and during treatment with Risperidone and appropriate preventive measures should be taken.
Intraoperative atonic iris syndrome (ISAR).
Intraoperative atonic iris syndrome has been observed during cataract surgery in patients treated with α1-adrenergic receptor antagonists, including risperidone.
ISAR increases the risk of complications during and after eye surgery. The ophthalmologist should be informed of any previous or current use of antipsychotic medications. The potential benefits of stopping α1-blocking medications before surgery have not been established; the risks of stopping antipsychotic medications should be weighed against the benefits.
Children.
Before prescribing Risperidone to children or adolescents with conduct disorder, the risk-benefit ratio should be carefully weighed, and the physical and social causes of aggressive behavior, such as painful stimuli or inappropriate responses to the environment, should be evaluated.
Risperidone is associated with a modest increase in body weight and body mass index (BMI). Baseline weight measurement is recommended before starting treatment and regular weight monitoring during treatment. Growth changes in long-term open-label extension studies were within the expected range for age. The effects of long-term risperidone treatment on puberty and growth have not been adequately studied.
Due to the potential effects of prolonged hyperprolactinemia on growth and puberty in children and adolescents, regular clinical monitoring of the patient's endocrine status may be necessary, including measurement of height, body weight, monitoring of puberty, menstrual cycle and other prolactin-dependent phenomena.
Results from a small postmarketing observational study showed that patients aged 8–16 years treated with risperidone were, on average, 3.0–4.8 cm taller than those treated with other antipsychotic drugs. The data from this study are insufficient to determine whether risperidone affects final adult height and whether the measurements are directly related to the effects of risperidone on bone growth, whether the disease itself affects bone growth, or whether this is a result of better disease control and, as a result, greater height retention.
During treatment with risperidone, the presence of extrapyramidal symptoms and other movement disorders should be monitored regularly.
For dosage for children, see the section “Method of administration and dosage”.
Excipients.
Risperidone oral solution contains benzoic acid (E 210). Increased bilirubin levels may lead to neonatal jaundice, which may progress to kernicterus (deposition of unconjugated bilirubin in the brain tissue).
Use during pregnancy or breastfeeding
Pregnancy.
Controlled studies in pregnant women have not been conducted. Although no teratogenic effects were observed in animal studies, other signs of reproductive toxicity were observed. The potential risk to humans is unknown.
Newborns whose mothers have used antipsychotics (including risperidone) during the last trimester of pregnancy are at risk of developing reversible extrapyramidal symptoms and/or dependence syndrome. Symptoms include agitation, unusually high or low muscle tone, tremor, drowsiness, respiratory distress, or feeding difficulties. These complications may vary in severity. Therefore, close monitoring of the newborn is necessary.
Risperidone is not recommended during pregnancy unless clearly necessary. If you need to stop taking Risperidone during pregnancy, this should not be done abruptly.
Breastfeeding.
In animal studies, risperidone and 9-hydroxyrisperidone were excreted in breast milk. There are observations that risperidone and 9-hydroxyrisperidone may also be excreted in human breast milk. There are no data on adverse reactions in breast-fed infants. Therefore, the benefits of breastfeeding should be weighed against the potential risks to the child.
Fertility.
Like other drugs that are dopamine D2 receptor antagonists, Risperidone increases prolactin levels.
Hyperprolactinemia can suppress the production of gonadotropin-releasing hormone in the hypothalamus, leading to decreased secretion of pituitary gonadotropins. This can have a negative impact on reproductive function in both women and men due to impaired gonadal steroidogenesis.
No relevant effects were observed in preclinical studies.
Ability to influence reaction speed when driving vehicles or other mechanisms
Risperidone may have minor or moderate influence on the ability to drive and use machines due to potential effects on the nervous system and visual organs (see section 4.8). During treatment, it is recommended to refrain from driving or operating machinery until the individual sensitivity of patients to the drug is known.
Method of administration and doses
Dosage.
Schizophrenia.
Adults.
Risperidone can be taken once or twice a day.
You should start taking 2 mg of Risperidone per day, and on the second day the dose can be increased to 4 mg. After that, the dose can be maintained unchanged or, if necessary, continue individual dose adjustment.
For most patients, the recommended dose is
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.













