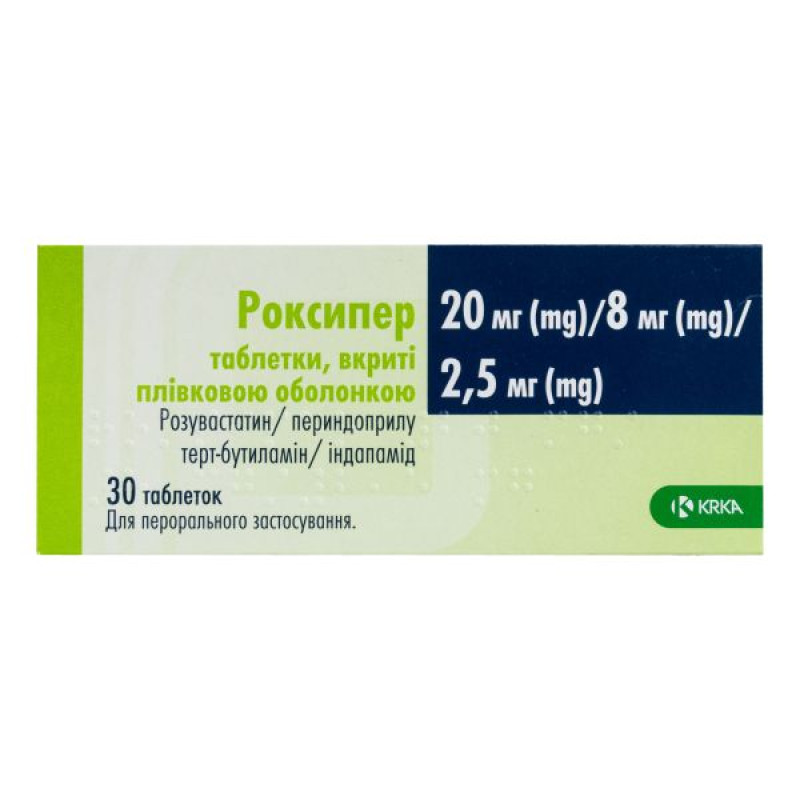
Roxiper film-coated tablets 20 mg/8 mg/2.5 mg No. 30

Instructions for Roxiper film-coated tablets 20 mg/8 mg/2.5 mg No. 30
Composition
active ingredients: rosuvastatin (as rosuvastatin calcium), perindopril tert-butylamine and indapamide;
1 tablet contains 10 mg of rosuvastatin (as rosuvastatin calcium), 4 mg of perindopril tert-butylamine and 1.25 mg of indapamide or
20 mg of rosuvastatin (as rosuvastatin calcium), 4 mg of perindopril tert-butylamine and 1.25 mg of indapamide, or
10 mg rosuvastatin (as rosuvastatin calcium), 8 mg perindopril tert-butylamine and 2.5 mg indapamide, or
20 mg of rosuvastatin (as rosuvastatin calcium), 8 mg of perindopril tert-butylamine and 2.5 mg of indapamide;
excipients: microcrystalline cellulose (type 112 and type 200, low moisture), crospovidone (type A), colloidal anhydrous silicon dioxide, magnesium stearate;
film coating: polyvinyl alcohol, macrogol 3350, titanium dioxide (E 171), talc, red iron oxide (E 172), black iron oxide (E 172)*, yellow iron oxide (E 172)*.
* Not contained in 10 mg/8 mg/2.5 mg tablets.
Dosage form
Film-coated tablets.
Main physicochemical properties:
10 mg/4 mg/1.25 mg
Reddish-brown, round, slightly biconvex, film-coated tablets with beveled edges, engraved with PIR1 on one side.
20 mg/4 mg/1.25 mg
Almost pink, round, slightly biconvex, film-coated tablets with beveled edges, engraved with the PIR2 symbol on one side.
10 mg/8 mg/2.5 mg
Light pink, round, slightly biconvex, film-coated tablets with beveled edges, engraved with PIR3 on one side.
20 mg/8 mg/2.5 mg
Pale pinkish-brown, round, slightly biconvex, film-coated tablets with beveled edges, engraved with the PIR4 symbol on one side.
Pharmacotherapeutic group
Hypolipidemic combined agents. HMG-CoA reductase inhibitors, other combinations. ATC code C10BX13.
Pharmacological properties
Roxipre is a combination of the tert-butylamine salt of perindopril, an angiotensin-converting enzyme (ACE) inhibitor, indapamide, a chlorosulfone diuretic, and rosuvastatin, a selective and competitive inhibitor of HMG-CoA reductase. The pharmacological properties are due to the properties of each of the components used separately, in addition to those associated with the additive synergistic effect of the combination of perindopril and indapamide.
Pharmacodynamics.
Mechanism of action
Perindopril
Perindopril is an ACE inhibitor that converts angiotensin I to angiotensin II, a vasoconstrictor, and also causes the breakdown of the vasodilator agent bradykinin to form an inactive heptapeptide.
ACE inhibition by perindopril leads to:
decreased aldosterone secretion;
increased plasma renin activity, as aldosterone no longer causes negative feedback;
reduction in total peripheral resistance with a predominant effect on the vascular bed in the muscles and kidneys, without concomitant salt and water retention or reflex tachycardia during chronic treatment.
Perindopril has an antihypertensive effect also in patients with low or normal renin concentrations.
Perindopril acts through the active metabolite, perindoprilat. Other metabolites are inactive.
Perindopril makes the heart work easier:
venodilator effect, probably due to changes in prostaglandin metabolism: reduction of preload;
reducing total peripheral vascular resistance: reducing afterload.
Studies conducted in patients with heart failure have shown:
decreased filling pressure of the left and right ventricles;
reduction in total peripheral vascular resistance;
increased cardiac output and improved cardiac index;
increased regional blood circulation in the muscles.
In addition, performance on exercise tests improves significantly.
Indapamide
Indapamide is a sulfonamide derivative with an indole ring, pharmacologically related to thiazide diuretics. Indapamide inhibits sodium reabsorption in the renal cortical segment. This increases the urinary excretion of sodium and chloride and, to a lesser extent, the excretion of potassium and magnesium, thereby increasing diuresis. This mechanism provides the antihypertensive effect.
Rosuvastatin
Rosuvastatin is a selective and competitive inhibitor of HMG-CoA reductase, the enzyme that converts 3-hydroxy-3-methylglutaryl-coenzyme A to mevalonate, a precursor of cholesterol. The primary site of action of rosuvastatin is the liver, the target organ for lowering cholesterol concentrations.
Rosuvastatin increases the number of hepatic low-density lipoprotein (LDL) receptors on the cell surface, increasing the uptake and catabolism of LDL, and leads to inhibition of hepatic synthesis of very low-density lipoprotein (VLDL), thereby reducing the total number of VLDL and LDL particles.
Pharmacodynamic effects
Related to perindopril/indapamide
This antihypertensive effect lasts for 24 hours. A decrease in blood pressure is achieved in less than a month without tachyphylaxis. Discontinuation of treatment is not accompanied by a withdrawal effect. Clinical studies have shown that the simultaneous administration of perindopril and indapamide causes a synergistic antihypertensive effect, which is the result of the effects of the individual components of the drug.
The multicenter, randomized, double-blind, open-label, controlled PICXEL study evaluated the effect of the perindopril/indapamide combination on left ventricular hypertrophy compared with enalapril monotherapy using ECG.
The study treated patients with hypertension and left ventricular hypertrophy (defined as left ventricular mass index (LVMI) > 120 g/m2 in men and > 100 g/m2 in women) with perindopril/indapamide 2 mg/0.625 mg or enalapril 10 mg once daily for 1 year. The dose of perindopril/indapamide 8 mg/2.5 mg or enalapril 40 mg once daily was adjusted according to blood pressure. 34% of patients were treated with perindopril/indapamide 2 mg/0.625 mg compared to 20% of patients taking enalapril 10 mg.
At the end of treatment, LVMI decreased most significantly in the perindopril/indapamide group (-10.1 g/m²) compared with the enalapril group (-1.1 g/m²) in all randomized subgroups of patients. The difference in LVMI between groups was -8.3 (95% confidence interval (CI) (-11.5,-5.0), p < 0.0001).
The best effect on LVEF was achieved with the combination of perindopril 8 mg/indapamide 2.5 mg.
The combination of perindopril/indapamide has been shown to reduce systolic and diastolic blood pressure in patients with hypertension: -5.8 mmHg (95% CI (-7.9, -3.7), p < 0.0001) for systolic blood pressure and -2.3 mmHg (95% CI (-3.6, -0.9), p = 0.0004) for diastolic blood pressure.
Related to perindopril
Perindopril effectively reduces blood pressure in patients with any degree of arterial hypertension: mild, moderate and severe. The reduction in systolic and diastolic blood pressure is observed both in the supine and standing positions. The maximum antihypertensive effect develops 4–6 hours after taking a single dose and persists for more than a day. Perindopril has a high level of final ACE inhibitor blockade (approximately 80%) 24 hours after administration.
In patients who responded to treatment, normalization of blood pressure occurs within a month and is maintained without the occurrence of tachyphylaxis.
Discontinuation of therapy is not accompanied by a withdrawal effect.
Perindopril has vasodilating properties, restores the elasticity of large arteries, corrects histomorphometric changes in arterial resistance and reduces left ventricular hypertrophy. Additional synergism develops when a thiazide diuretic is added, if necessary.
The combination of an ACE inhibitor and a thiazide diuretic reduces the risk of hypokalemia, which can occur when a diuretic is prescribed as monotherapy.
Clinical trial data with dual blockade of the renin-angiotensin-aldosterone system (RAAS)
The concomitant use of ACE inhibitors and angiotensin II receptor blockers has been investigated in two large-scale randomized controlled trials [ONTARGET (ONgoing Telmisartan Alone and Ramipril Global Endpoint Trial) and VA NEPHRON-D (The Veterans Affairs Nephropathy in Diabetes)].
ONTARGET is a study in patients with a history of cardiovascular or cerebrovascular disease or type 2 diabetes mellitus with evidence of target organ damage. VA NEPHRON-D is a study in patients with type 2 diabetes mellitus and diabetic nephropathy.
The studies did not show a significant beneficial effect for patients with renal and/or cardiovascular diseases and on mortality from them, while compared with monotherapy there was an increased risk of hyperkalemia, acute kidney injury and/or hypotension. Given the similarity of pharmacodynamic properties, these results are also applicable to other ACE inhibitors and angiotensin II receptor blockers.
Concomitant use of ACE inhibitors and angiotensin II receptor blockers is contraindicated in patients with diabetic nephropathy.
ALTITUDE (Aliskiren in Type 2 Diabetes with Cardiovascular and Renal Endpoints) is a study of the treatment benefits of adding aliskiren to standard therapy with an ACE inhibitor or an angiotensin II receptor blocker in patients with type 2 diabetes and/or chronic kidney disease, cardiovascular disease. The study was stopped early due to an increased risk of adverse events. Cardiovascular mortality, stroke, and reports of adverse events and serious complications (hyperkalemia, hypotension, or renal dysfunction) were more frequent in the aliskiren group compared with the placebo group.
Related to indapamide
The antihypertensive effect of indapamide as monotherapy lasts for 24 hours. This effect is manifested at doses in which the diuretic properties are minimal.
The antihypertensive effect of indapamide is associated with improved arterial elasticity and a decrease in arteriolar resistance and total peripheral vascular resistance.
When the recommended dose is exceeded, the therapeutic effect of thiazide and thiazide-like diuretics does not increase, while the number of undesirable effects increases. If the treatment is not effective enough, it is not recommended to increase the dose.
In addition, as shown in studies of varying duration in patients with hypertension, indapamide:
does not affect the metabolism of lipids: triglycerides, LDL and high-density lipoproteins (HDL);
does not affect carbohydrate metabolism, even in patients with hypertension and diabetes.
Associated with rosuvastatin
Rosuvastatin reduces elevated LDL-cholesterol (LDL-C), total cholesterol (TC), and triglycerides and increases HDL-C concentrations. It also significantly reduces apolipoprotein B, low-density lipoprotein cholesterol (LDL-C), VLDL-C, VLDL-triglycerides, and increases apolipoprotein A-I concentrations. Rosuvastatin also reduces the LDL-C/HDL-C, TC/HDL-C, and LDL-C/HDL-C ratios, as well as apolipoprotein B/apolipoprotein A-I.
The therapeutic effect is achieved within 1 week after the start of treatment, and 90% of the maximum treatment effect is achieved after 2 weeks. The maximum effect is usually achieved after 4 weeks and is maintained throughout the course of treatment.
Rosuvastatin is effective in adults with hypercholesterolemia, with or without hypertriglyceridemia, regardless of race, sex, or age, and in specific patient groups, such as those with diabetes or familial hypercholesterolemia.
Pooled phase III data showed the efficacy of rosuvastatin in the treatment of the majority of patients with type IIa and IIb hypercholesterolemia (mean baseline LDL-C >4.8 mmol/L) according to the targets recognized by the European Atherosclerosis Society (EAS; 1998): more than 80% of patients treated with a dose of 10 mg achieved target LDL-C levels (<3 mmol/L).
In a large study of 435 patients with heterozygous familial hypercholesterolemia, rosuvastatin was administered in doses ranging from 20 mg to 80 mg with intensive titration. All doses had beneficial effects on lipid parameters and treatment. After titration to a daily dose of 40 mg (12 weeks of treatment), LDL-C was reduced by 53%. 33% of patients achieved the EAS target for LDL-C levels (< 3 mmol/L).
An open-label study of 42 patients with homozygous familial hypercholesterolemia evaluated the effect of rosuvastatin 20–40 mg with intensive titration. In the overall group, the mean reduction in LDL-C reached 22%.
In clinical studies with a limited number of patients, rosuvastatin had an additive effect on lowering triglycerides when used in combination with fenofibrate and increasing HDL-C levels when used in combination with niacin (see section "Special warnings and precautions for use").
In a multicenter, double-blind, placebo-controlled clinical trial (METEOR), 984 patients aged 45 to 70 years with low risk of cardiovascular disease (CVD) (defined as Framingham risk < 10% after 10 years) and a mean LDL-C level of 4.0 mmol/L (154.5 mg/dL) but with subclinical atherosclerosis [detected by intima-media thickness (IMT)] received 40 mg of rosuvastatin once daily for 2 years. Rosuvastatin significantly reduced the rate of progression of maximum IMT thickness for 12 carotid artery sites compared with placebo by -0.0145 mm/year [95% confidence interval -0.0196, -0.0093; p < 0.0001]. The change from baseline was -0.0014 mm/year [-0.12%/year (nonsignificant)] for rosuvastatin, compared with a progression of +0.0131 mm/year [1.12%/year (p < 0.0001)] for placebo. No direct correlation was established between IMD thickness and a reduction in the risk of cardiovascular events. The population included in the METEOR study was at low risk of CVD and did not represent the target population for rosuvastatin 40 mg. The 40 mg dose should be administered to patients with severe hypercholesterolemia and high cardiovascular risk (see section 4.2).
The JUPITER study evaluated the effect of rosuvastatin on the occurrence of major atherosclerotic cardiovascular complications in 17,802 men (≥ 50 years) and women (≥ 60 years).
Study participants were randomized (randomly divided) to receive placebo (n = 8901) or rosuvastatin 20 mg per day (n = 8901) for an average of 2 years.
LDL-C concentrations decreased by 45% (p < 0.001) in the rosuvastatin group compared with the placebo group.
In the JUPITER study, the number of subjects who discontinued study drug due to an adverse reaction was 6.6% among those taking rosuvastatin and 6.2% among those taking placebo. The most common adverse reactions leading to discontinuation were: myalgia (0.3% rosuvastatin, 0.2% placebo), abdominal pain (0.03% rosuvastatin, 0.02% placebo), and rash (0.02% rosuvastatin, 0.03% placebo). The most common adverse reactions that occurred more frequently or at the same rate as placebo were: urinary tract infection (8.7% in the rosuvastatin group, 8.6% in the placebo group), nasopharyngitis (7.6% in the rosuvastatin group, 7.2% in the placebo group), back pain (7.6% in the rosuvastatin group, 6.9% in the placebo group) and myalgia (7.6% in the rosuvastatin group, 6.6% in the placebo group).
Pharmacokinetics.
Perindopril
Absorption and bioavailability
After oral administration, perindopril is rapidly absorbed, with peak plasma concentrations occurring within 1 hour. The plasma half-life of perindopril is 1 hour.
Distribution
The volume of distribution of free perindopril is approximately 0.2 l/kg. The protein binding of perindopril to plasma proteins is 20%, especially to ACE, but is concentration-dependent.
Metabolism
Perindopril is a prodrug. 27% of the total amount of perindopril absorbed is converted to the active metabolite perindoprilat. In addition, five more inactive metabolites are formed. The maximum concentration of perindoprilat in the blood plasma is reached within 3–4 hours.
Since the presence of food in the stomach leads to a decrease in the conversion of perindopril to perindoprilat and, therefore, to a decrease in bioavailability, perindopril should be administered orally in the morning before meals.
Breeding
Perindoprilat is excreted in the urine, and the half-life of the unbound fraction is approximately 17 hours, resulting in a steady state within 4 days.
Linearity/nonlinearity
A linear relationship between the dose of perindopril and its plasma concentration has been demonstrated.
Elderly patients
In the elderly and patients with heart or kidney failure, the excretion of perindoprilat is reduced.
Kidney dysfunction
In case of impaired renal function, it is recommended to change the dose depending on the degree of impairment (creatinine clearance).
Perindoprilat is removed from the circulation by dialysis, its clearance is 70 ml/min.
Cirrhosis
In liver cirrhosis, the kinetics of perindopril change, with the hepatic clearance of the parent molecule being halved, but the amount of perindoprilat formed does not change, so the dose of the drug may not be changed in this disease (see sections “Method of administration and dosage” and “Special precautions for use”).
Indapamide
Absorption
Indapamide is released rapidly and almost completely absorbed from the gastrointestinal tract.
The maximum concentration of indapamide in the blood serum is reached approximately 1 hour after taking the drug.
Distribution
The binding of indapamide to blood plasma proteins is 79%.
Breeding
The plasma half-life is 14 to 24 hours (average 18 hours). Regular administration of the drug does not lead to accumulation of indapamide. 70% of indapamide is excreted mainly by the kidneys and 22% is excreted with feces in the form of inactive metabolites.
Kidney failure
The pharmacokinetic parameters of the drug are unchanged in patients with renal impairment.
Rosuvastatin
Absorption
Peak plasma concentrations of rosuvastatin are reached approximately 5 hours after oral administration. Absolute bioavailability is approximately 20%.
Distribution
Rosuvastatin is extensively metabolized in the liver, which is the primary site of cholesterol synthesis and LDL-C clearance. The volume of distribution of rosuvastatin is approximately 134 L. Approximately 90% of rosuvastatin is bound to plasma proteins, primarily albumin.
Metabolism
Rosuvastatin undergoes limited metabolism (approximately 10%). In vitro metabolism studies using human hepatocytes indicate that rosuvastatin undergoes only minimal P450-mediated metabolism, which is of no clinical significance. CYP2C9 was the major isoenzyme involved in metabolism, with 2C19, 3A4 and 2D6 being involved to a lesser extent. The main metabolites identified are the N-desmethyl and lactone metabolites. The N-desmethyl metabolite is approximately 50% less active than rosuvastatin, the lactone form is considered clinically inactive. Rosuvastatin has more than 90% inhibitory activity against HMG-CoA reductase circulating in the general circulation.
Breeding
Approximately 90% of a rosuvastatin dose is excreted unchanged in the feces (consisting of absorbed and unabsorbed active substance), and the remainder is excreted in the urine. Approximately 5% is excreted unchanged in the urine. The plasma half-life is approximately 20 hours. The half-life does not increase with high dosage. The geometric mean plasma clearance is approximately 50 liters per hour (coefficient of variation 21.7%). As with other HMG-CoA reductase inhibitors, hepatic uptake of rosuvastatin involves the membrane transporter OATP-C. This transporter is important for the elimination of rosuvastatin from the liver.
Systemic exposure to rosuvastatin increases in proportion to the dose. There is no change in pharmacokinetic parameters after multiple daily administration.
Age and gender
The pharmacokinetics of rosuvastatin in adults were not significantly affected by age or gender. The pharmacokinetics of rosuvastatin in children and adolescents with heterozygous familial hypercholesterolemia are similar to or lower than those in adult volunteers (see the Children section below).
Race
Pharmacokinetic studies demonstrate an approximately 2-fold increase in AUC and Cmax of rosuvastatin in patients of Asian origin (Japanese, Chinese, Filipinos, Vietnamese and Koreans) compared with patients of the Caucasian race; in Indians, an approximately 1.3-fold increase in mean AUC and Cmax values is observed. Pharmacokinetic analysis of the patient group did not reveal any clinically significant differences in pharmacokinetics between representatives of the Caucasian and Negroid races.
Kidney dysfunction
In a study involving patients with varying degrees of renal impairment, mild to moderate renal disease had no effect on the plasma concentrations of rosuvastatin or the N-desmethyl metabolite. In patients with severe renal impairment (creatinine clearance < 30 ml/min), plasma concentrations increased 3-fold and the N-desmethyl metabolite concentrations increased 9-fold compared with healthy volunteers. Steady-state plasma concentrations of rosuvastatin in patients undergoing hemodialysis were approximately 50% higher than in healthy volunteers.
Liver dysfunction
In a study of patients with varying degrees of hepatic impairment, there was no evidence of increased exposure to rosuvastatin in patients with Child-Pugh scores of 7 or less. However, at least a 2-fold increase in systemic exposure was observed in two patients with Child-Pugh scores of 8 and 9.
Genetic polymorphisms
The distribution of HMG-CoA reductase inhibitors, including rosuvastatin, involves the transport proteins OATP1B1 and BCRP. Patients with genetic polymorphisms of SLCO1B1 (OATP1B1) and/or ABCG2 (BCRP) are at risk of increased exposure to rosuvastatin. The individual polymorphisms SLCO1B1 c.521CC and ABCG2 c.421AA are associated with higher exposure to rosuvastatin (AUC) compared to the genotypes SLCO1B1 c.521TT or ABCG2 c.421CC. These individual genotypes have not been established in clinical practice, but a lower daily dose of rosuvastatin is recommended for patients with these types of polymorphisms.
Children
Pharmacokinetic parameters in children aged 10 to 17 years with heterozygous familial hypercholesterolemia have not been fully characterized. A small pharmacokinetic study in 18 children showed that the exposure of rosuvastatin (tablets) in children is comparable to that in adults. No significant deviation from dose proportionality is expected.
Indication
Roxipre is indicated for replacement therapy in severe hypertension and the presence of one of the following factors: primary hypercholesterolemia (type IIa, including heterozygous familial hypercholesterolemia), mixed dyslipidemia (type IIb) or heterozygous familial hypercholesterolemia, in adults whose condition is adequately controlled with rosuvastatin, perindopril and indapamide, when used simultaneously in the same doses as in the combination.
Contraindication
Associated with rosuvastatin
Hypersensitivity to rosuvastatin.
Active liver disease, including of unknown etiology, persistent elevation of serum transaminases, and elevation of any serum transaminase to more than 3 times the upper limit of normal.
Myopathy.
Concomitant use of cyclosporine.
Pregnancy and breastfeeding. Also contraindicated in women of reproductive age who are not using appropriate contraception.
Related to perindopril:
Hypersensitivity to perindopril or any other ACE inhibitor.
History of angioedema associated with previous treatment with ACE inhibitors.
Hereditary or idiopathic angioedema.
II or III trimester of pregnancy (see sections "Special precautions for use" and "Use during pregnancy or breastfeeding").
Concomitant administration with drugs containing the active substance aliskiren to patients with diabetes mellitus or patients with renal insufficiency (glomerular filtration rate < 60 ml/min/1.73 m2) (see sections “Pharmacodynamics” and “Interaction with other medicinal products and other types of interactions”).
Concomitant use with sacubitril/valsartan: Therapy with the drug should be initiated no earlier than 36 hours after the last dose of sacubitril/valsartan (see sections “Interaction with other medicinal products and other types of interactions” and “Special precautions for use”).
Extracorporeal treatments that result in blood coming into contact with negatively charged surfaces (see section “Interaction with other medicinal products and other types of interactions”).
Significant bilateral renal artery stenosis or stenosis of the artery to a single functioning kidney (see section "Special warnings and precautions for use").
Related to indapamide:
Hypersensitivity to indapamide or any other sulfonamide.
Hepatic encephalopathy.
Severe liver failure.
Use in combination with non-antiarrhythmic drugs that cause torsades de pointes (see section "Interaction with other medicinal products and other types of interactions").
Breastfeeding (see section "Use during pregnancy or breastfeeding").
Contraindications for the use of the drug:
All contraindications associated with each of the components and hypersensitivity to any excipient of the medicinal product.
Severe renal failure (creatinine clearance < 30 ml/min).
Due to lack of relevant therapeutic data, Roxiper should not be used:
Dialysis patients.
Patients with untreated heart failure.
Interaction with other medicinal products and other types of interactions
Related to perindopril and indapamide
Concomitant use not recommended
Lithium
When lithium is used concomitantly with ACE inhibitors, reversible increases in serum lithium concentrations and signs of toxicity have been observed. Concomitant use of thiazide diuretics further increases the risk of lithium toxicity when using ACE inhibitors. The combination of indapamide and lithium is not recommended, but if combination therapy is necessary, careful monitoring of serum lithium levels should be performed (see section "Special warnings and precautions for use").
Concomitant use requiring special precautions
Baclofen
Increased antihypertensive effect. Blood pressure and renal function should be monitored and the dosage adjusted if necessary.
Nonsteroidal anti-inflammatory drugs (NSAIDs) (including high doses of acetylsalicylic acid)
NSAIDs (including acetylsalicylic acid at anti-inflammatory doses, cyclooxygenase-2 inhibitors and non-selective NSAIDs) may reduce the antihypertensive effect of ACE inhibitors. In addition, NSAIDs and ACE inhibitors additionally increase serum potassium levels, which may lead to deterioration of renal function, including acute renal failure, especially in patients with impaired renal function. The combination should be used with caution, especially in elderly patients. Patients should be adequately hydrated and consideration should be given to monitoring renal function after initiation of concomitant therapy and periodically thereafter.
Concomitant use requiring monitoring
Imipramine-like antidepressants (tricyclics), neuroleptics: increased hypotensive effect and increased risk of orthostatic hypotension (additive effect).
Corticosteroids, tetracosactide: reduction of hypotensive effect (salt and water retention under the influence of corticosteroids).
Other antihypertensive agents: the use of other antihypertensive agents with the combination of perindopril/indapamide may lead to an additive blood pressure-lowering effect.
Related to perindopril
Clinical trial data suggest that dual blockade of the RAAS by concomitant administration of ACE inhibitors, angiotensin II receptor blockers or aliskiren is associated with a higher incidence of adverse reactions such as hypotension, hyperkalaemia and decreased renal function (including acute renal failure) compared with the use of a single drug affecting the RAAS (see sections 5.1, 5.3 and 4.4).
Drugs that cause hyperkalemia
Some medicinal products or therapeutic classes of medicinal products may cause hyperkalaemia: aliskiren, potassium salts, potassium-sparing diuretics, ACE inhibitors, angiotensin II receptor antagonists, NSAIDs, heparins, immunosuppressants such as ciclosporin or tacrolimus, trimethoprim, co-trimoxazole (trimethoprim/sulfamethoxazole). Concomitant use of these medicinal products increases the risk of hyperkalaemia.
Concomitant use is contraindicated
Aliskiren: In patients with diabetes mellitus or patients with impaired renal function, the risk of hyperkalemia, worsening of renal function, and cardiovascular morbidity and mortality is increased.
Extracorporeal treatments that result in contact of blood with negatively charged surfaces, such as high-flux membranes for dialysis or hemofiltration (e.g. polyacrylic membranes) and for low-density lipoprotein apheresis with dextran sulfate, increase the risk of severe anaphylactoid reactions (see section 4.3). If such treatment is necessary, consideration should be given to using a different type of dialysis membrane or a different class of antihypertensive drug.
Sacubitril/Valsartan
Concomitant use of perindopril with sacubitril/valsartan is contraindicated, as concomitant use of ACE inhibitors and sacubitril/valsartan increases the risk of angioedema. Sacubitril/valsartan should not be initiated earlier than 36 hours after the last dose of perindopril. Perindopril therapy should not be initiated earlier than 36 hours after the last dose of sacubitril/valsartan (see sections 4.3 and 4.4).
Aliskiren: in all other patients, as well as in patients with diabetes mellitus or patients with impaired renal function, the risk of hyperkalemia, worsening of renal function and cardiovascular morbidity and mortality is increased (see section "Special warnings and precautions for use").
Concomitant use of ACE inhibitors and angiotensin receptor blockers
Published data indicate that in patients with atherosclerosis, heart failure or diabetes mellitus with target organ damage, the simultaneous use of ACE inhibitors and angiotensin receptor blockers was accompanied by an increased incidence of arterial hypotension, syncope, hyperkalemia and deterioration of renal function (including acute renal failure) compared with those with monotherapy with drugs that affect the RAAS. Dual blockade (i.e. the combination of an ACE inhibitor with angiotensin II receptor antagonists) may be used in selected cases with careful monitoring of renal function, potassium levels and blood pressure (see section "Special instructions").
Estramustine
The risk of adverse reactions such as angioedema increases.
Potassium-sparing diuretics (spironolactone, triamterene, alone or in combination), potassium supplements, or potassium-containing salt substitutes
Although potassium is usually within normal limits, hyperkalaemia may occur in some patients receiving perindopril. Potassium-sparing diuretics (e.g. spironolactone, triamterene or amiloride), potassium supplements or potassium-containing salt substitutes may lead to significant increases in serum potassium. Caution should also be exercised when perindopril is administered concomitantly with other agents that increase serum potassium, such as trimethoprim and co-trimoxazole (trimethoprim/sulfamethoxazole), since trimethoprim is known to act as a potassium-sparing diuretic to amiloride. Therefore, concomitant use of perindopril with the above-mentioned drugs is not recommended. However, if concomitant administration of the above-mentioned substances is necessary, they should be used with caution and with close monitoring of plasma potassium levels.
Co-trimoxazole (trimethoprim/sulfamethoxazole)
Patients receiving concomitant co-trimoxazole (trimethoprim/sulfamethoxazole) are at increased risk of hyperkalemia (see section 4.4).
Concomitant use requiring special precautions
Antidiabetic drugs (insulin, hypoglycemic sulfonamides - with captopril and enalapril)
Epidemiological studies have shown that the concomitant use of ACE inhibitors and antidiabetic agents (insulins, oral hypoglycemic agents) may lead to an increased blood glucose-lowering effect with a risk of hypoglycemia. This phenomenon was more likely during the first weeks of combined treatment and in patients with impaired renal function.
Diuretics
In patients taking diuretics, and especially in those with impaired water and electrolyte metabolism, an excessive decrease in blood pressure is possible after starting treatment with an ACE inhibitor. The likelihood of developing a hypotensive effect is reduced by discontinuing the diuretic, increasing the circulating blood volume or salt intake before starting therapy with perindopril. Treatment should be started with low doses and gradually increased.
In hypertension, when a previously prescribed diuretic may have caused water/electrolyte depletion, it should be discontinued before starting treatment.
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.