Seretide Evohaler inhalation aerosol 25 mcg/250 mcg 120 doses

Instructions for Seretide Evohaler inhalation aerosol 25 mcg/250 mcg 120 doses
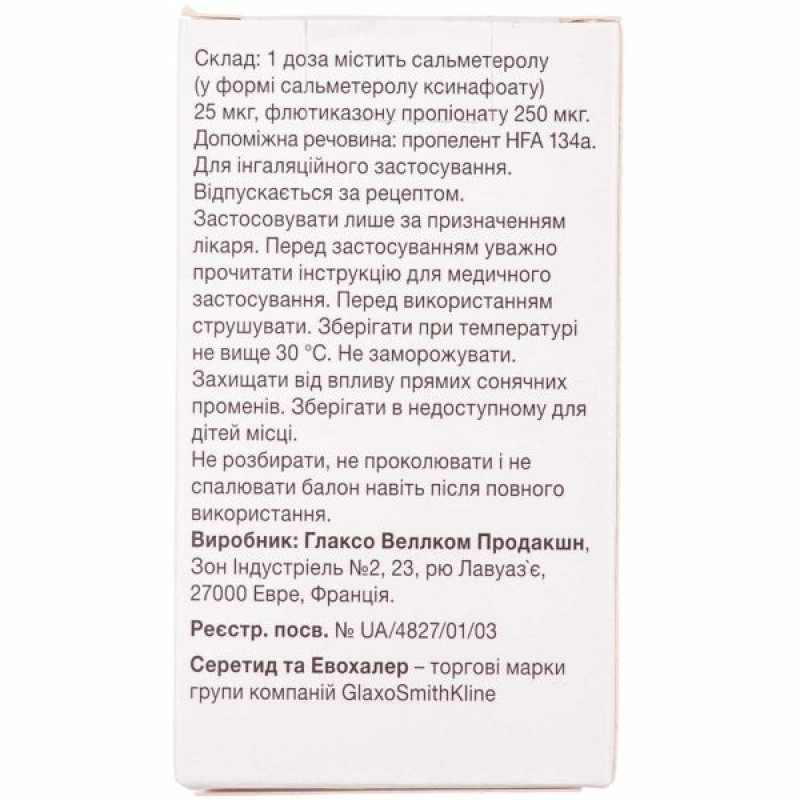
Composition
active ingredients: salmeterol (in the form of salmeterol xinafoate), fluticasone propionate;
1 dose of the drug contains 25 mcg of salmeterol (in the form of salmeterol xinafoate) and 50 mcg or 125 mcg, or 250 mcg of fluticasone propionate;
excipient: propellant HFA 134a.
Dosage form
Inhalation aerosol, metered.
Main physicochemical properties: white or almost white suspension.
Pharmacotherapeutic group
Antiasthmatics. Adrenergic drugs for inhalation use. Adrenergic drugs in combination with corticosteroids or other drugs, except anticholinergics. Salmeterol and fluticasone. ATX code R03A K06.
Pharmacological properties
Pharmacodynamics.
Seretide Evohaler contains salmeterol and fluticasone propionate, which have different mechanisms of action.
Salmeterol
Salmeterol is a long-acting (12 hours) selective b2-adrenoceptor agonist that has a long side chain linked to the external domain of the receptor.
Salmeterol provides longer-lasting bronchodilation (at least 12 hours) than recommended doses of traditional short-acting b2-adrenergic agonists.
Fluticasone propionate
Fluticasone propionate, when used by inhalation in recommended doses, has a pronounced glucocorticoid anti-inflammatory effect in the lungs, which leads to a reduction in clinical symptoms and the frequency of exacerbations of bronchial asthma without the occurrence of adverse reactions observed with systemic use of corticosteroids.
Pharmacokinetics.
When salmeterol and fluticasone propionate are used together by inhalation, the pharmacokinetics of each component remain the same as when these components are used separately, therefore their pharmacokinetic characteristics are presented separately.
Salmeterol
Salmeterol acts locally in the lung tissue, so its plasma levels do not correlate with the therapeutic effect. In addition, data on the pharmacokinetics of salmeterol are limited because of the technical difficulties in determining the very low plasma concentrations of the drug (approximately 200 picograms/mL or less) after inhalation at therapeutic doses.
Fluticasone propionate
The absolute bioavailability of fluticasone propionate after inhalation in healthy volunteers is approximately 5-11% of the nominal dose, depending on the inhalation device used. In patients with bronchial asthma, lower levels of systemic exposure are observed with inhaled fluticasone propionate. Systemic absorption occurs mainly in the lungs, initially rapidly, then slowing down. Part of the inhaled dose may be swallowed, but its systemic effect is minimal due to the poor solubility of fluticasone propionate in water and extensive first-pass metabolism in the liver. The bioavailability of fluticasone propionate when absorbed from the gastrointestinal tract is less than 1%. There is a linear increase in systemic exposure to fluticasone propionate with increasing inhaled dose of the drug. The distribution of fluticasone propionate is characterized by high plasma clearance (1150 ml/min), a large volume of distribution (approximately 300 l) and a terminal half-life of approximately 8 hours. The degree of binding to plasma proteins is relatively high (91%). Fluticasone propionate is rapidly eliminated from the systemic circulation, mainly by metabolism to an inactive carboxyl metabolite by the cytochrome P450 enzyme CYP3A4. Other unidentified metabolites are excreted in the feces. Renal clearance of fluticasone propionate is very low, with less than 5% of the dose excreted in the urine, mainly as metabolites. The majority of the dose is excreted in the feces as metabolites and unchanged drug.
Indication
Regular treatment of bronchial asthma in patients for whom combination therapy with a long-acting b2-agonist and an inhaled corticosteroid is indicated:
patients with inadequate control of bronchial asthma on the background of therapy with inhaled corticosteroids and short-acting b2-agonists on demand or
patients with adequate control of bronchial asthma on therapy with inhaled corticosteroids and long-acting b2-agonists in various inhalers.
Contraindication
Hypersensitivity to any component of the drug.
Interaction with other medicinal products and other types of interactions
adrenoblockers may weaken or eliminate the effect of salmeterol. Nonselective and selective beta-blockers should be avoided in patients with asthma, unless there are serious reasons for this. The use of b2-agonists can cause potentially dangerous hypokalemia. The drug is prescribed with particular caution to patients with acute severe asthma, since the simultaneous use of xanthine derivatives, steroids and diuretics may increase adverse reactions.
Concomitant use with medicinal products containing other b-adrenergic agents may have a potential additive effect.
Under normal conditions, low plasma concentrations of fluticasone propionate are achieved after inhalation administration due to extensive first-pass metabolism and high systemic clearance of the drug mediated by cytochrome CYP3A4 in the liver and intestine. Therefore, the likelihood of clinically significant drug interactions due to fluticasone propionate is very low.
In a drug interaction study in healthy volunteers with intranasal fluticasone propionate, ritonavir (a potent inhibitor of cytochrome CYP3A4) at a dose of 100 mg twice daily increased the plasma concentration of fluticasone propionate several hundred-fold, resulting in a significant decrease in serum cortisol. No data are available for inhaled fluticasone propionate, but a significant increase in serum fluticasone propionate levels is expected. Cases of Cushing's syndrome and adrenal suppression have been reported. Concomitant use should be avoided unless the benefit outweighs the potential risk of systemic glucocorticoid adverse reactions.
In a small interaction study with the less potent CYP3A inhibitor ketoconazole in healthy volunteers, fluticasone propionate exposure was increased by 150% after 1 inhalation, resulting in a greater reduction in plasma cortisol levels compared to fluticasone propionate alone. Co-administration with other potent CYP3A inhibitors such as itraconazole, cobicistat-containing products and moderate CYP3A inhibitors such as erythromycin is expected to increase systemic exposure to fluticasone propionate and the risk of systemic adverse reactions.
Such combinations should be avoided unless the expected benefit outweighs the potential risk of systemic corticosteroid adverse reactions. In such cases, patients should be monitored for the development of systemic adverse events.
Salmeterol.
Strong CYP3A4 inhibitors
Concomitant administration of ketoconazole (400 mg orally once daily) and salmeterol (50 mcg inhaled twice daily) in 15 healthy volunteers for 7 days resulted in a significant increase in plasma salmeterol exposure (1.4-fold for maximum concentration (Cmax) and 15-fold for area under the concentration-time curve (AUC)). This may lead to an increased incidence of other systemic reactions to salmeterol (e.g. QT prolongation and palpitations) compared to salmeterol or ketoconazole alone (see section 4.4).
No clinically significant effects on blood pressure, heart rate, blood glucose, or blood potassium were observed. Co-administration with ketoconazole did not increase the half-life of salmeterol or the accumulation of salmeterol with repeated administration.
Concomitant use with ketoconazole should be avoided unless the expected benefit outweighs the potential risk of systemic adverse reactions to salmeterol. There is likely to be a similar risk of interaction with other strong CYPA4 inhibitors (e.g. itraconazole, telithromycin, ritonavir).
Moderate CYP3A4 inhibitors
Co-administration of erythromycin (500 mg orally 3 times a day) and salmeterol (50 mcg inhaled 2 times a day) in 15 healthy volunteers for 6 days resulted in a small and statistically insignificant increase in plasma salmeterol exposure (1.4-fold Cmax and 1.2-fold AUC). Co-administration with erythromycin was not associated with any serious adverse reactions.
Application features
Seretide Evohaler is not a treatment for acute symptoms requiring rapid and short-acting bronchodilators (e.g. salbutamol). The patient should be advised to carry a reliever with them at all times.
Seretide Evohaler treatment should not be initiated during an exacerbation of the disease, in case of significant or acute deterioration of the patient's condition and course of the disease.
Serious asthma-related adverse reactions and exacerbations may occur during treatment with Seretide Evohaler. Patients should be advised to continue treatment but to seek medical advice if these symptoms remain uncontrolled or worsen after starting treatment with Seretide Evohaler.
Increased use of short-acting bronchodilators to relieve asthma symptoms or decreased response to such drugs indicates worsening asthma control and requires medical consultation. Rapid and progressive deterioration of asthma control is potentially life-threatening and requires urgent medical attention. An increase in the dose of corticosteroids should be considered. The patient should also be examined by a doctor if the prescribed dose of Seretide Evohaler does not provide adequate control of asthma symptoms.
Treatment with the drug should not be stopped suddenly, as this may lead to a worsening of the disease. The dose should be gradually reduced under the supervision of a doctor.
As with any inhaled corticosteroid, Seretide Evohaler should be used with caution in patients with active or latent pulmonary tuberculosis, fungal, viral or other respiratory tract infections. In such cases, appropriate treatment should be initiated immediately, if necessary.
Cardiovascular effects such as increases in systolic blood pressure and heart rate may occur with all sympathomimetic drugs, especially at high doses. Therefore, the drug should be used with caution in patients with cardiovascular disease.
The use of high therapeutic doses of Seretide Evohaler may rarely cause cardiac arrhythmias, such as supraventricular tachycardia, extrasystoles or atrial fibrillation, as well as a mild transient decrease in serum potassium. Therefore, the drug should be used with caution in patients with severe cardiovascular disease, cardiac arrhythmias, diabetes mellitus, thyrotoxicosis, patients with uncorrected hypokalemia or those prone to low serum potassium.
There have been very rare reports of increased blood glucose levels (see section 4.8). This should be taken into account when prescribing the drug to patients with a history of diabetes.
As with other inhaled medications, paradoxical bronchospasm with sudden increase in dyspnea after inhalation may occur. Appropriate treatment with a rapid-acting, short-acting inhaled bronchodilator should be initiated immediately. Seretide Evohaler should be discontinued immediately, the patient assessed and, if necessary, alternative therapy instituted.
Pharmacological side effects of β2-agonist treatment, such as tremor, palpitations and headache, have been reported, but these are transient and decrease with regular therapy (see section “Adverse reactions”).
Systemic effects may occur with inhaled corticosteroids, especially at high doses for long periods. These effects are much less likely to occur than with oral corticosteroids. Possible systemic effects include Cushing's syndrome, Cushingoid features, adrenal suppression, decreased bone mineralization, cataracts and glaucoma, and, less commonly, a range of physiological and behavioral reactions, including psychomotor hyperactivity, sleep disturbances, restlessness, depression and aggression (especially in children). It is therefore important to monitor the patient's condition and reduce the dose of inhaled corticosteroid to the minimum effective dose sufficient to control the symptoms of bronchial asthma.
Long-term therapy with high doses of inhaled corticosteroids may cause adrenal suppression and acute adrenal crisis. Isolated cases of adrenal suppression and acute adrenal crisis have been reported with doses of fluticasone propionate from 500 mcg to 1000 mcg. Situations that may potentially precipitate acute adrenal crisis include trauma, surgery, infection or any rapid dose reduction. Symptoms are usually vague and may include anorexia, abdominal pain, weight loss, fatigue, headache, nausea, vomiting, hypotension, decreased level of consciousness, hypoglycaemia and convulsions. During periods of stress or during surgery, the need for additional systemic corticosteroids should be considered because of the potential for adrenal suppression.
Systemic absorption of salmeterol and fluticasone propionate occurs primarily through the lungs. Since the use of a spacer device with an inhaler may increase the delivery of the drug to the lungs, it should be noted that this increases the risk of systemic adverse reactions. Single-dose pharmacokinetic studies have shown that systemic exposure to salmeterol and fluticasone propionate may increase by 2-fold with the use of the AeroChamber Plus spacer device compared to the Volumatic spacer device.
The use of inhaled fluticasone propionate should minimise the need for oral steroids, but patients who are transferred from oral steroids for a period of time may still be at risk of developing impaired adrenal reserve. Therefore, such patients should be treated with special care and with regular monitoring of adrenal function. Patients who have used high doses of corticosteroids as emergency treatment in the past are also at risk. The possibility of residual insufficiency should always be borne in mind in emergency situations and possible stressful situations and the need for corticosteroids should be taken into account (see section 4.8). Special advice may be required before certain procedures to assess the degree of adrenal insufficiency.
When starting inhaled fluticasone propionate, withdrawal of systemic treatment should be gradual. Patients should be advised to carry a steroid alert card at all times, indicating the possible need for additional therapy in a stressful situation.
Ritonavir may significantly increase the plasma concentrations of fluticasone propionate. Therefore, concomitant use of these drugs should be avoided unless the expected benefit to the patient outweighs the potential risk of systemic corticosteroid adverse reactions. The risk of systemic adverse reactions is also increased when fluticasone propionate is used concomitantly with other potent inhibitors of cytochrome CYP3A.
A three-year clinical trial in patients with chronic obstructive pulmonary disease (COPD) showed an increased incidence of lower respiratory tract infections (mainly pneumonia and bronchitis) with the combination of salmeterol and fluticasone propionate using the Diskus delivery device compared to placebo. In the three-year study in COPD patients, older patients, patients with a low body mass index (< 25 kg/m2) and patients with very severe disease (FEV1 < 30% predicted) were also at higher risk of developing pneumonia regardless of treatment. Physicians should be aware of the possibility of pneumonia or other lower respiratory tract infections in patients with COPD, as the clinical symptoms of pneumonia and exacerbations of COPD often overlap. If pneumonia develops in a patient with severe COPD, treatment with Seretide Evohaler should be reconsidered. The safety and efficacy of Seretide Evohaler in patients with COPD have not been established, therefore Seretide Evohaler is not prescribed to patients with COPD.
Concomitant use with systemic ketoconazole significantly increases systemic exposure to salmeterol, which may lead to an increased incidence of systemic adverse reactions (e.g. QT prolongation and palpitations). Therefore, concomitant use with ketoconazole and other strong CYP3A inhibitors should be avoided unless the expected benefit outweighs the potential risk of systemic adverse reactions to salmeterol (see section 4.5).
Vision impairment
Visual impairment may occur with systemic and topical corticosteroids. If a patient presents with symptoms such as blurred vision or other visual disturbances, they should be referred to an ophthalmologist for evaluation of possible causes, including cataracts, glaucoma, or rare conditions such as central serous chorioretinopathy, which have been reported with systemic and topical corticosteroids.
Children
Children and adolescents under 16 years of age receiving high doses of fluticasone propionate (usually ≥ 1000 mcg/day) are at particular risk of developing systemic adverse reactions. Systemic reactions may occur mainly with long-term high-dose therapy. Possible systemic effects include Cushing's syndrome, Cushingoid features, adrenal suppression, acute adrenal crisis, growth retardation in children and adolescents, and less commonly, mental and behavioral disorders including psychomotor hyperactivity, sleep disorders, anxiety, depression, or aggression.
It is recommended that growth be monitored regularly in children receiving inhaled corticosteroids for long periods of time. The dose of inhaled corticosteroids should be reduced to the lowest effective dose sufficient to control asthma symptoms.
Use during pregnancy or breastfeeding
Pregnancy
Extensive data on the use of Seretide Evohaler in pregnant women (more than 1000 cases) have shown no evidence of impaired embryonic development or toxic effects on the fetus and newborn.
Results of a retrospective epidemiological study did not reveal an increased risk of major congenital malformations after exposure to fluticasone propionate during the first trimester of pregnancy compared with other inhaled corticosteroids.
Reproductive toxicity has been observed in animal studies following administration of β2-adrenergic agonists and glucocorticosteroids.
Seretide Evohaler should be used during pregnancy only if the expected benefit to the woman clearly outweighs the potential risk to the fetus. For the treatment of pregnant women, the lowest effective dose of fluticasone propionate necessary to provide adequate control of asthma symptoms should be prescribed.
Breast-feeding
It is not known whether salmeterol and fluticasone propionate, as well as their metabolites, are excreted in human milk.
Studies in rats have shown that salmeterol, fluticasone propionate and their metabolites are excreted in human milk. Therefore, a risk to the breast-fed infant cannot be excluded during maternal treatment with this drug. A decision should be made whether to discontinue breast-feeding or to discontinue Seretide Evohaler taking into account the benefit of breast-feeding to the child and the expected benefit of therapy to the mother.
There are no data on the effects on human fertility. Animal studies have not shown any effect of salmeterol or fluticasone propionate on fertility.
Ability to influence reaction speed when driving vehicles or other mechanisms
Seretide Evohaler has no or negligible influence on the ability to drive and use machines.
Method of administration and doses
Seretide Evohaler is for inhalation use only.
Patients should be aware that Seretide Evohaler must be used regularly, even when there are no asthma attacks.
Patients should be regularly reviewed to ensure that the dose selected for them remains optimally effective, which can only be changed by the doctor. The dose of the drug should be titrated to the minimum effective dose that provides control of the disease symptoms. If such effective control is achieved against the background of the minimum effective dose of the drug when used twice a day, the next step may be to transfer the patient to the use of a single inhaled corticosteroid. As an alternative, for the treatment of patients who require the use of long-acting b2-agonists, the dose of Seretide Evohaler can be reduced to 1 dose per day if, in the opinion of the doctor, this will adequately maintain control of the disease symptoms. If the patient has a history of nocturnal asthma attacks, this single dose should be used at bedtime. If the history of attacks mainly occurred during the day, the dose should be used in the morning.
The amount of fluticasone propionate in the selected formulation of Seretide Evohaler should be appropriate for the severity of the disease. Note: Seretide Evohaler 25 mcg/50 mcg is not appropriate for the treatment of adults and children with severe asthma. If an individual patient requires dosages that exceed the recommended regimen, the necessary doses of b2-agonist and/or corticosteroid should be prescribed.
Recommended doses.
Adults and adolescents aged 12 years and over:
2 inhalations of 25 mcg salmeterol/50 mcg fluticasone propionate twice daily
or 2 inhalations of 25 mcg salmeterol/125 mcg fluticasone propionate 2 times a day;
or 2 inhalations of 25 mcg salmeterol/250 mcg fluticasone propionate 2 times daily.
For the treatment of adults and adolescents with moderate persistent asthma (daily symptoms, daily use of quick-relief medication and moderate to severe airflow limitation), Seretide Evohaler can be used as initial maintenance therapy when rapid control of symptoms is required. In such cases, the recommended starting dose is 2 inhalations of 25 micrograms salmeterol/50 micrograms fluticasone propionate twice daily. Once asthma symptoms are controlled, consideration should be given to reducing the volume of therapy by one step and to using only the inhaled corticosteroid. When reducing the volume of therapy by one step, it is important to review the patient regularly.
In the absence of one or two severity criteria, no clear advantage of Seretide Evohaler over inhaled fluticasone propionate alone as initial maintenance therapy has been demonstrated. In general, inhaled corticosteroids remain the first-line treatment for most patients. Seretide Evohaler should not be used as initial therapy for mild asthma. Seretide Evohaler 25 mcg/50 mcg is not appropriate for the treatment of adults and children with severe asthma. For the treatment of patients with severe asthma, it is recommended that an appropriate dose of inhaled corticosteroid is first established before any fixed combination is used.
Children.
Children aged 4–12 years:
2 inhalations of 25 mcg salmeterol/50 mcg fluticasone propionate twice daily.
The maximum daily dose of fluticasone propionate in Seretide Evohaler is 100 mcg twice a day.
There are no data on the use of Seretide Evohaler in children under 4 years of age.
Special patient groups.
There is no need to adjust the dose in elderly patients or patients with renal insufficiency. There are no data on the use of Seretide Evohaler in patients with hepatic insufficiency.
Instructions for using the inhaler
Patients should be advised on the proper use of the inhaler. Inhalation should be performed while standing or sitting. This inhaler is specifically designed for use in an upright position.
Checking the inhaler
Before using the inhaler for the first time or after a break in use for more than 1 week, remove the mouthpiece cap by lightly pressing on it from the sides, shake the inhaler well and spray 2 times into the air to make sure it is working properly.
Using an inhaler
Remove the mouthpiece cap by pressing lightly on the sides.
Make sure that there are no foreign objects inside and outside the inhaler, including the mouthpiece.
Shake the inhaler thoroughly to remove any foreign object from the inhaler and to ensure that the contents of the inhaler are evenly mixed.
Take the deepest possible exhalation, then place the mouthpiece between your teeth and cover it with your lips without biting.
While breathing in through your mouth, press the top of the inhaler to spray the medicine, while continuing to breathe in slowly and deeply. 1 press on the top of the inhaler corresponds to 1 dose.
Hold your breath, remove the inhaler from your mouth and remove your finger from the top of the inhaler. Continue to hold your breath for as long as possible.
If further sprays are required, wait approximately 30 seconds, holding the inhaler upright. Then follow steps 3–7.
Afterwards, rinse your mouth with water and spit it out.
Snap the mouthpiece cap into place by pressing in the desired direction until it clicks.
IMPORTANTLY
Perform the steps described in points 5, 6 and 7 without rushing. Before spraying, inhale as slowly as possible. The first few times you should practice in front of a mirror. If a "cloud" appears near the top of the inhaler or on the sides of your mouth, you must start the procedure again from point 3.
Immediately after use, close the mouthpiece with the cap by gently pressing it until it clicks. Do not apply excessive force when pressing.
Rinsing the mouth, spitting water and/or brushing the teeth after each use of the medicine minimizes the risk of developing oropharyngeal candidiasis and hoarseness.
As with other inhaled medications, therapeutic efficacy may be reduced when the canister is cooled.
The cylinder contains a liquid under pressure. Do not heat above 50 °C, protect from direct sunlight. Do not disassemble, puncture or burn the cylinder, even after complete use.
Disposal of unused medicinal product or used containers should be carried out in accordance with local requirements.
If your doctor has given you other instructions for using your inhaler, you should follow them and seek advice if you have any difficulties.
Children.
It may be necessary for children to be given inhalations by an adult. Ask the child to exhale and spray immediately after they start to inhale. It is recommended to learn the technique together. Older children or frail adults can hold the inhaler with both hands. Place both index fingers on the top of the inhaler and both thumbs on the base below the mouthpiece.
Cleaning
The inhaler should be cleaned at least once a week.
Remove the mouthpiece cap.
Do not remove the metal cylinder from the plastic case.
Wipe the outer and inner surfaces of the mouthpiece cap and plastic case with a dry cloth.
Place the mouthpiece cap in place until it clicks, without applying excessive force.
DO NOT PUT THE METAL BALLOON IN WATER.
Children.
There is no data on the use of Seretide Evohaler in children under 4 years of age, therefore the use of the drug in this age group is not recommended.
Overdose
There is no information from clinical studies on cases of overdose with Seretide Evohaler, however, data on overdose of both active substances are provided below.
Signs and symptoms to be expected in case of salmeterol overdose are typical of overstimulation by β2-agonists, including dizziness, tremor, headache, tachycardia, increased systolic blood pressure. If Seretide Evohaler treatment has to be discontinued as a result of overdose of the β2-agonist contained in the product, appropriate steroid replacement therapy should be prescribed. In addition, hypokalemia may occur, therefore serum potassium levels should be monitored and the need for potassium replacement therapy should be considered.
Acute overdose
Inhalation of fluticasone propionate in doses exceeding those recommended may cause temporary suppression of adrenal function. This does not require immediate action, as adrenal function recovers within a few days, which can be verified by measuring plasma cortisol.
Chronic overdose
There is a risk of adrenal suppression when using higher than approved doses of Seretide Evohaler for a long time.
Acute adrenal crisis has been reported very rarely, occurring mainly in children treated with higher than recommended doses for prolonged periods (several months or years). Hypoglycaemia associated with confusion and convulsions has been observed. Factors that may potentially precipitate acute adrenal crisis include trauma, surgery, infection and any rapid reduction in the dose of inhaled fluticasone propionate.
Monitoring of adrenal reserve is recommended. In the event of an overdose of fluticasone propionate with Seretide Evohaler, therapy can be continued at appropriate doses to control symptoms.
There is no specific treatment for overdose of salmeterol and fluticasone propionate; supportive therapy with monitoring of the patient's condition is necessary.
Side effects
Since Seretide Evohaler contains salmeterol and fluticasone propionate, adverse reactions of the type and severity characteristic of each component can be expected. Additional adverse reactions due to the simultaneous use of the two components have not been observed.
Adverse reactions associated with the use of salmeterol/fluticasone propionate are listed below (table) and classified by organ system and frequency of occurrence. The frequency is defined as: very common (≥ 1/10), common (≥ 1/100 and < 1/10), uncommon (≥ 1/1,000 and < 1/100), rare (≥ 1/10,000 and < 1/1,000) and unknown (cannot be estimated from the available data). Information on the frequency of occurrence is obtained from the results of clinical trials. Information on cases recorded in the placebo group has not been taken into account.
| Organs and organ systems | Side effect | Frequency |
| Infections and infestations | Candidiasis of the mucous membranes of the mouth and throat Pneumonia Bronchitis Esophageal candidiasis | Often Often1.3 Often1.3 Rarely |
On the part of the immune system | Hypersensitivity reactions: skin hypersensitivity reactions, angioedema (mainly of the face and oropharynx), respiratory symptoms (shortness of breath), respiratory symptoms (bronchospasm), anaphylactic reactions, including anaphylactic shock | Infrequently Rarely Infrequently Rarely Rarely |
| From the endocrine system | Cushing's syndrome, Cushingoid symptoms, adrenal suppression, growth retardation in children and adolescents, decreased bone mineralization | Rarely4 |
| Metabolism and digestive disorders | Hypokalemia Hyperglycemia | Often3, 4 Infrequently |
| Mental disorders | Trouble Sleep disturbances Behavioral changes, including psychomotor hyperactivity and irritability (predominantly in children) Depression, aggression (mainly in children) | Infrequently Infrequently Rarely Unknown |
| From the nervous system | Headache Tremor | Very often1 Infrequently |
| From the organs of vision | Cataract glaucoma Visual impairment | Infrequently Rarely4 Unknown4 |
| From the heart | Increased heartbeat Tachycardia Cardiac arrhythmia (including supraventricular tachycardia and extrasystole) atrial fibrillation Angina pectoris | Infrequently Infrequently Rarely Infrequently Infrequently |
| Respiratory system | Nasopharyngitis Throat irritation Hoarseness/dysphonia Sinusitis Paradoxical bronchospasm | Very often2,3 Often Often Often1.3 Rarely4 |
| Skin and subcutaneous tissue disorders | Bruises | Often1.3 |
| Musculoskeletal and connective tissue disorders | Muscle spasms Traumatic fractures Arthralgias Myalgia | Often Often Often Often |
1Reported as “common” in the placebo group.
2Reported as “very common” in the placebo group.
3Were recorded over 3 years during the COPD study.
4See chap.
There are no reviews for this product.
There are no reviews for this product, be the first to leave your review.
No questions about this product, be the first and ask your question.