Teronred film-coated tablets 250 mg No. 120

Instructions for Teronred film-coated tablets 250 mg No. 120
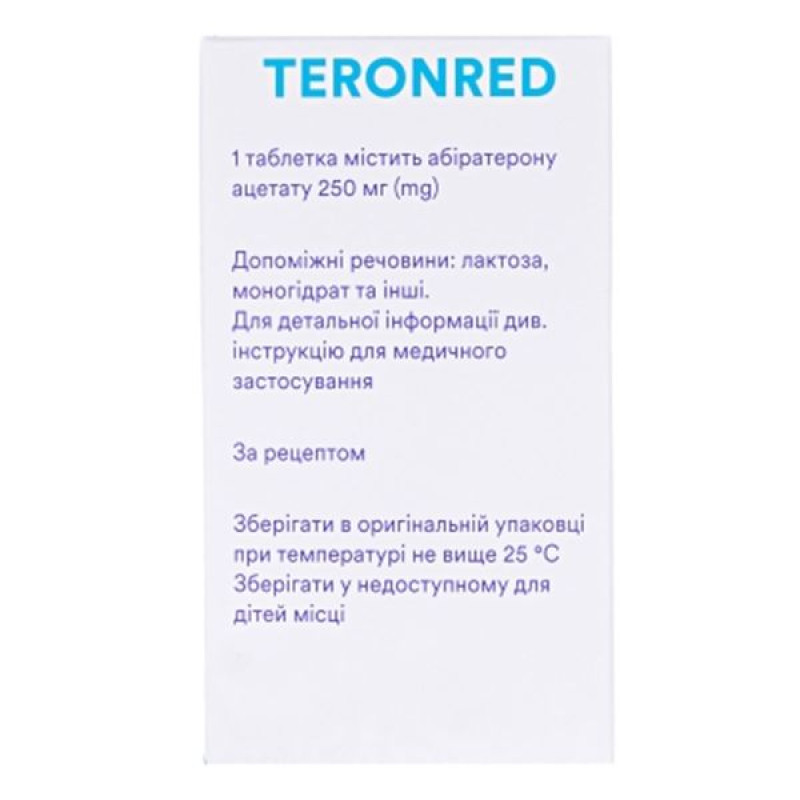
Composition
active ingredient: abiraterone acetate;
1 tablet contains abiraterone acetate 250 mg;
excipients: lactose monohydrate; microcrystalline cellulose; croscarmellose sodium; povidone; sodium lauryl sulfate; colloidal anhydrous silica; magnesium stearate; film coating Opadry White OY-58900 (film coating composition: hypromellose, titanium dioxide (E 171), polyethylene glycol).
Dosage form
Film-coated tablets.
Main physicochemical properties: biconvex, oval-shaped tablets, film-coated, white or almost white in color, engraved with "358" on one side and the company logo on the other side.
Pharmacotherapeutic group
Antineoplastic and immunomodulatory agents. Agents used for hormonal therapy. Hormone antagonists and similar agents. Other hormone antagonists and similar agents. Abiraterone. ATC code L02B X03.
Pharmacological properties
Pharmacodynamics.
Mechanism of action.
Abiraterone acetate is metabolized in vivo to abiraterone, which is an inhibitor of androgen biosynthesis. In particular, abiraterone selectively inhibits the enzyme 17α-hydroxylase/C17,20-lyase (CYP17). This enzyme is required for androgen biosynthesis in testicular tissues, adrenal cortex, and prostate tumors. CYP17 catalyzes the conversion of pregnenolone and progesterone to the precursors of testosterone, dehydroepiandrosterone (DHEA), and androstenedione, respectively, via 17α-hydroxylation and cleavage of the C17,20 bond. Inhibition of CYP17 also leads to increased production of mineralocorticoids by the adrenal glands (see section "Special warnings and precautions for use").
Androgen-sensitive prostate cancer responds to androgen-depleting treatments. However, androgen-depleting therapies, such as luteinizing hormone-releasing hormone (LH) agonists or orchiectomy, reduce testicular androgen production but do not affect adrenal or tumor androgen production. Treatment with abiraterone acetate reduces serum testosterone levels to undetectable levels when used concomitantly with LH agonists (or orchiectomy).
Pharmacodynamics.
The drug reduces serum testosterone and other androgens to a greater extent than LHRH agonists or orchiectomy. This is due to selective inhibition of CYP17, which is required for androgen biosynthesis. Prostate-specific antigen (PSA) is a biomarker in patients with prostate cancer. In a phase III clinical trial in patients who had failed taxane chemotherapy, patients treated with abiraterone acetate (38%) had a PSA reduction of at least 50% from baseline compared with patients treated with placebo (10%).
Pharmacokinetics.
The pharmacokinetics of abiraterone and abiraterone acetate have been studied in healthy volunteers, patients with metastatic prostate cancer, and non-cancer patients with hepatic or renal impairment. Abiraterone acetate is rapidly metabolized in vivo to abiraterone, which is an inhibitor of androgen biosynthesis.
Absorption.
After oral administration of abiraterone acetate in the fasting state, peak plasma concentrations are reached after 2 hours.
Administration of abiraterone acetate with food, compared to administration in the fasted state, results in a 10-fold increase in AUC and an almost 17-fold increase in Cmax of abiraterone relative to the mean systemic exposure to abiraterone, depending on the fat content of the meal. Therefore, administration with food has the potential to alter the systemic exposure of the drug. Therefore, the drug should not be taken with food, but should be administered at least 1 hour before or 2 hours after a meal. The tablets should be swallowed whole with sufficient liquid (see section 4.2).
Distribution.
The binding of 14C-abiraterone to human plasma proteins is 99.8%. The volume of distribution is approximately 5630 L, indicating that abiraterone is widely distributed in peripheral tissues.
Biotransformation.
Following oral administration of 14C-abiraterone acetate in abiraterone capsules, the acetate is hydrolyzed to abiraterone, which is further sulfated, hydroxylated, and oxidized primarily by the liver. The majority of circulating radioactivity (approximately 92%) is found as abiraterone metabolites. Of the 15 detectable metabolites, the two major metabolites, abiraterone sulfate and abiraterone sulfate N-oxide, each account for approximately 43% of the total radioactivity.
Breeding.
The mean plasma half-life of abiraterone is approximately 15 hours based on data from healthy volunteers. Following oral administration of 1000 mg of 14C-abiraterone acetate, approximately 88% of the radioactive dose is excreted in the feces and approximately 5% in the urine. The major compounds recovered in the feces are unchanged abiraterone acetate and abiraterone (approximately 55% and 22% of the administered dose, respectively).
The pharmacokinetics of abiraterone acetate were evaluated in patients with a history of mild or moderate hepatic impairment (Child-Pugh class A and B, respectively) and in healthy controls. The systemic exposure of abiraterone following a single oral dose of 1000 mg was increased by approximately 11% and 260% in patients with mild and moderate hepatic impairment, respectively. The mean elimination half-life of abiraterone was prolonged to approximately 18 hours in patients with mild hepatic impairment and to approximately 19 hours in patients with moderate hepatic impairment.
In another study, the pharmacokinetics of abiraterone were studied in patients (n = 8) with pre-existing severe hepatic impairment (Child-Pugh Class C) and in 8 healthy volunteers with normal hepatic function. Compared with healthy volunteers, in patients with severe hepatic impairment, systemic exposure (AUC) to abiraterone was increased by 600% and the unbound fraction by 80%.
No dose adjustment is required for patients with mild hepatic impairment.
The drug should be used with caution in patients with moderate hepatic impairment and only if the benefits of treatment outweigh the potential risks (see sections "Method of administration and dosage" and "Special warnings and precautions for use"). Abiraterone acetate should not be used in patients with severe hepatic impairment (see sections "Method of administration and dosage", "Contraindications" and "Special warnings and precautions for use").
Patients who develop hepatotoxicity during treatment may require treatment interruption and dose adjustment (see sections 4.2 and 4.4).
Patients with renal failure.
The pharmacokinetics of abiraterone acetate were compared in patients with end-stage renal disease on continuous hemodialysis and in a control group of patients with normal renal function. Systemic exposure to abiraterone after a single oral dose of 1000 mg was not increased in patients with end-stage renal disease on hemodialysis. There is no need to reduce the dose when using the drug in patients with renal insufficiency, including severe renal insufficiency. However, caution should be exercised when prescribing the drug to patients with prostate cancer with severe renal insufficiency, since clinical data on the use of abiraterone acetate in such patients are lacking.
Indication
The drug Teronred is indicated for use in combination with prednisone or prednisolone for the treatment of:
- metastatic castration-resistant prostate cancer (CRPC) with asymptomatic or mild course in adult men after unsatisfactory results of androgen deprivation therapy, and for whom chemotherapy is not clinically indicated;
- metastatic castration-resistant prostate cancer (MRCP) in adult men whose disease has progressed during or after prior chemotherapy with docetaxel.
Contraindication
- hypersensitivity to the active substance or to excipients;
- pregnancy and reproductive age in women;
- severe hepatic insufficiency (Child-Pugh class C) (see sections “Method of administration and dosage”, “Special instructions for use” and “Pharmacokinetics”).
- Teronred with prednisone or prednisolone is contraindicated in combination with Ra-223.
Interaction with other medicinal products and other types of interactions
Effect of food on abiraterone acetate.
The use of Teronred with food significantly increases the absorption of abiraterone acetate. The efficacy and safety of the drug with food have not been established, therefore this medicinal product should not be taken with food (see sections “Method of administration and dosage” and “Pharmacokinetics”).
Interaction with other drugs.
In a pharmacokinetic interaction study in healthy volunteers who initially administered rifampicin, a potent CYP3A4 inducer, at a dose of 600 mg daily for 6 days followed by a single dose of 1000 mg abiraterone acetate, the mean plasma AUC of abiraterone was decreased by 55%.
Strong CYP3A4 inducers (e.g. phenytoin, carbamazepine, rifampicin, rifabutin, rifapentine, phenobarbital, St. John's wort [Hypericum perforatum]) should be avoided during treatment with Teronred, unless there is no therapeutic alternative.
In a separate clinical study in healthy volunteers, concomitant use of ketoconazole, a strong CYP3A4 inhibitor, had no clinically important effect on the pharmacokinetics of abiraterone.
Effects on other medicines.
It is recommended to use Teronred with caution with drugs that are activated or metabolized by CYP2D6, in particular with drugs that have a narrow therapeutic index. Therefore, a dose reduction of the drug that is metabolized by CYP2D6 and has a narrow therapeutic index should be considered. Such drugs include metoprolol, propranolol, desipramine, venlafaxine, haloperidol, risperidone, propafenone, flecainide, codeine, oxycodone, tramadol (the last three require CYP2D6 to form active analgesic metabolites).
In a CYP2C8 drug interaction study in healthy volunteers, administration of pioglitazone with a single dose of 1000 mg abiraterone acetate increased the AUC of pioglitazone by 46% and decreased the AUC of each of the active metabolites of pioglitazone M-III and M-IV by 10%. Although these results indicate that there is no clinically relevant effect of co-administration of Teronred with drugs that are primarily metabolized by CYP2C8, patients should be closely monitored for signs of toxicity associated with the concomitant use of CYP2C8 substrates with a narrow therapeutic index.
The major metabolites of abiraterone, abiraterone sulfate and abiraterone sulfate N-oxide, have been shown to inhibit the OATP1B1 transporter in vitro. This may result in increased concentrations of drugs excreted by OATP1B1. There are no clinical data to support transporter-dependent interactions.
Drugs that prolong the QT interval.
Since androgen deprivation therapy may lead to QT prolongation, Teronred should be used with caution with drugs that may prolong the QT interval or with drugs that may induce torsades de pointes, such as class IA (e.g. quinidine, disopyramide) or class III (e.g. amiodarone, sotalol, dofetilide, ibutilide) antiarrhythmics, methadone, moxifloxacin, antipsychotics, etc. (see section "Special warnings and precautions for use").
Use with spironolactone.
Spironolactone binds to androgen receptors, which may lead to increased levels of prostate-specific antigen (PSA). Concomitant use with Teronred is not recommended.
Application features
Arterial hypertension, hypokalemia, fluid retention, and heart failure due to excess mineralocorticoids.
Teronred may cause hypertension, hypokalemia and fluid retention (see section "Adverse reactions") due to increased mineralocorticoid levels resulting from CYP17 inhibition. Concomitant use of corticosteroids suppresses the activity of adrenocorticotropic hormone (ACTH), which leads to a decrease in the frequency and severity of these side effects. The drug should be used with caution in patients in whom exacerbation of the underlying disease may be manifested by increased blood pressure, hypokalemia (on the background of taking cardiac glycosides) or fluid retention, for example, in heart failure, severe or unstable angina, recent myocardial infarction or ventricular arrhythmia, and patients with severe renal failure.
Before starting treatment, patients at high risk of developing congestive heart failure (e.g., heart failure, uncontrolled hypertension, or history of ischemic heart disease) should have their cardiac function assessed (e.g., echocardiogram). Heart failure should be treated and cardiac function optimized before starting therapy with Teronred. Hypertension, hypokalemia, and fluid retention should be monitored. Blood pressure, potassium levels, fluid retention (weight gain, peripheral edema), and other manifestations of congestive heart failure should be measured every 2 weeks during treatment for the first 3 months and monthly thereafter. Abnormalities should be corrected. In patients who developed hypokalemia while receiving Teronred, QT prolongation has been observed. In case of clinically significant abnormalities in cardiac function, appropriate therapy should be administered and, if necessary, discontinuation of treatment with the drug should be considered (see section “Method of administration and dosage”).
Hepatotoxicity and liver failure.
During clinical trials, cases of marked elevations in liver enzymes have been reported, requiring discontinuation of treatment or dose adjustment of the drug (see section "Adverse reactions"). Serum transaminase levels should be monitored before the use of Teronred, as well as every two weeks during the first three months of treatment, and then monthly. In the event of the development of clinical symptoms or signs indicating the development of hepatotoxicity, serum transaminase levels should be determined immediately. If the level of hepatic transaminases - alanine transaminase (ALT) and aspartate transaminase (AST) exceeds the upper limit of normal by more than 5 times, treatment with Teronred should be discontinued immediately and liver function should be carefully assessed. Treatment with a reduced dose of Teronred can be resumed only if the patient's liver function has normalized to the initial level (see section "Method of administration and dosage").
In case of severe hepatotoxicity (ALT or AST levels 20 times the upper limit of normal), the drug should be discontinued and further administration of abiraterone should be avoided.
Patients with active viral hepatitis were not included in clinical trials, therefore there are no data on the use of abiraterone acetate in this population.
There are no data on the safety and efficacy of multiple doses of abiraterone acetate in patients with moderate or severe hepatic impairment (Child-Pugh Class B or C). The drug should be used with caution in patients with moderate hepatic impairment and only if the benefits of treatment significantly outweigh the potential risks (see sections 4.2 and 4.3). The drug should not be used in patients with severe hepatic impairment (see sections 4.2 and 4.4).
In the post-marketing period, rare cases of acute hepatic failure and fulminant hepatitis, some of which were fatal, have been reported (see section 4.8).
Withdrawal of corticosteroids and localization of stressful situations.
If prednisone or prednisolone is discontinued, the patient should be carefully monitored for signs of adrenal insufficiency. If Teronred is continued after corticosteroids have been discontinued, the patient should be monitored for mineralocorticoid excess.
If a patient has experienced a severe stressful situation, they may be prescribed increased doses of prednisone or prednisolone during and after the stressful situation.
Bone density.
In men with metastatic prostate cancer (castration-resistant prostate cancer), a decrease in bone density is possible. The use of Teronred in combination with glucocorticosteroids may enhance this effect.
Previous use of ketoconazole.
Lower susceptibility rates to Teronred can be expected in patients who have previously received ketoconazole.
Hyperglycemia.
The use of corticosteroids may increase hyperglycemia, so patients with diabetes should monitor their blood sugar levels frequently.
Use with chemotherapy.
The safety and efficacy of concomitant use of Teronred with cytotoxic chemotherapy have not been established.
Intolerance to excipients.
The medicinal product contains lactose. Patients with hereditary galactose intolerance, lactase deficiency or glucose-galactose malabsorption syndrome should not take Teronred. The medicinal product contains more than 1.18 mmol (or 27 mg) of sodium per dose of 4 tablets, which should be taken into account by patients on a controlled sodium diet.
Potential risks.
Men with metastatic castration-resistant prostate cancer, including those receiving Teronred therapy, may experience anemia and sexual dysfunction.
Myopathy and rhabdomyolysis have been reported in patients receiving Teronred. Most of these events occurred within the first 6 months of treatment and resolved after discontinuation of the drug. Caution should be exercised when Teronred is used concomitantly with drugs associated with the development of myopathy or rhabdomyolysis.
Interaction with other drugs.
The concomitant use of Teronred with strong CYP3A4 inducers should be avoided due to the risk of decreased systemic exposure to abiraterone, unless there is no therapeutic alternative (see section 4.5).
Combination of abiraterone and prednisone/prednisolone with Ra-223.
Treatment with abiraterone and prednisone/prednisolone in combination with Ra-223 is contraindicated (see Contraindications) due to an increased risk of fractures and a trend towards increased mortality in patients with asymptomatic or mildly symptomatic prostate cancer observed in clinical trials.
It is not recommended to start further treatment with Ra-223 earlier than 5 days after the last dose of Teronred in combination with prednisone/prednisolone.
Use during pregnancy or breastfeeding
Women of reproductive age.
There are no data on the use of the drug during pregnancy. This drug is contraindicated in women who may potentially become pregnant.
Contraception in men and women.
There are no data on the presence of abiraterone or its metabolites in semen. A condom should be used during sexual intercourse with a pregnant woman. If the patient is sexually active with a woman of reproductive age, a condom should be used in combination with other effective methods of contraception. Animal studies have shown reproductive toxicity.
Pregnancy.
Teronred is not indicated for use in women. Abiraterone acetate is contraindicated in pregnant women and women of childbearing potential.
Lactation period.
Teronred is not used in women.
Fertility.
Abiraterone affected the fertility of animals in studies, but this effect was reversible.
Ability to influence reaction speed when driving vehicles or other mechanisms
Teronred has no or negligible influence on the ability to drive and use machines.
Method of administration and doses
The drug should be taken on an empty stomach (at least 2 hours after a meal, and food should also be avoided for 1 hour after taking the drug). The tablet is taken whole, without chewing or crushing. It is recommended to drink water.
Dosage.
The recommended dose is 1000 mg (4 tablets of 250 mg) as a single daily dose, the drug should not be taken with food. Taking the drug with food increases the systemic exposure of abiraterone.
Dosage of prednisone and prednisolone.
The recommended dose of prednisone or prednisolone for the treatment of metastatic castration-resistant prostate cancer in combination with Teronred is 10 mg per day.
Patients who have not undergone surgical castration should continue medical castration with an LHRH analogue during treatment with Teronred.
Serum transaminase levels should be monitored before initiating treatment with abiraterone, every two weeks for the first three months of treatment, and monthly thereafter. Blood pressure, serum potassium, and fluid retention should be monitored monthly. Patients at high risk of congestive heart failure should be monitored every two weeks for the first three months of treatment, and monthly thereafter (see section 4.4).
Patients with a history of hypokalemia or who develop hypokalemia during treatment with Teronred should maintain potassium levels ≥ 4.0 mM.
Patients who develop Grade ≥ 3 toxicity, including hypertension, hypokalemia, edema, and other non-mineralocorticoid toxicities, should discontinue treatment and initiate appropriate treatment. Teronred treatment should only be resumed after symptoms of toxicity have resolved to Grade 1 or resolved.
If a daily dose of both Teronred and prednisone or prednisolone is missed, treatment should be resumed the next day using the usual daily dose.
Hepatotoxicity.
If a patient develops severe hepatotoxicity (ALT or AST levels exceeding 20 times the upper limit of normal) while taking the drug, abiraterone treatment should be discontinued and not resumed.
Liver failure.
No dose adjustment is required in patients with a history of Child-Pugh Class A hepatic impairment.
Moderate hepatic impairment (Child-Pugh Class B) has been shown to increase the systemic exposure of abiraterone administered orally at a dose of 1000 mg once daily by four-fold. There are no data on the clinical safety and efficacy of multiple doses of abiraterone acetate in patients with moderate or severe hepatic impairment (Child-Pugh Class B or C). No dose adjustment is anticipated. The use of Teronred in patients with moderate hepatic impairment should be carefully considered: the benefits of treatment should significantly outweigh the potential risks. Teronred should not be used in patients with severe hepatic impairment.
Kidney failure.
Patients with renal insufficiency do not require dose adjustment of abiraterone. There is no clinical experience with the drug in patients with prostate cancer and severe renal insufficiency. Caution should be exercised when using abiraterone in this category of patients.
Children.
The drug Teronred is not intended for use in children.
Overdose
Experience with overdose of Teronred is limited. There is no specific antidote. Therefore, in case of overdose, the drug should be discontinued and symptomatic treatment and monitoring for arrhythmias, hypokalemia and symptoms of fluid retention should be administered. Liver function should also be assessed.
Adverse reactions
In a pooled analysis of adverse reactions observed in the Phase 3 studies with abiraterone with an incidence of ≥ 10%, peripheral edema, hypokalemia, hypertension, and urinary tract infections, increased alanine aminotransferase and/or aspartate aminotransferase levels were reported. Other important adverse reactions included cardiac disorders, hepatotoxicity, bone fractures, and allergic alveolitis.
Abiraterone may cause hypertension, hypokalemia, and fluid retention, which is a consequence of its mechanism of action. In clinical trials, expected mineralocorticoid adverse reactions were observed more frequently in patients receiving the drug than in patients receiving placebo: hypokalemia - 18% vs. 8%, hypertension - 22% vs. 16%, and fluid retention (peripheral edema) - 23% vs. 17%, respectively. In patients treated with the drug, hypokalemia grade 3 and 4 on the CTCAE (version 4.0) adverse reaction scale was observed in 6% and 2% of patients, respectively, hypertension - 8% and 5% of patients, respectively, and fluid retention (peripheral edema) - 1% and 1% of patients, respectively. Mineralocorticoid reactions can usually be successfully corrected with medical treatment. Concomitant administration of corticosteroids reduces the frequency and severity of these adverse reactions (see section "Special warnings and precautions for use").
In studies of patients with metastatic prostate cancer who were using an LHRH analogue or who had undergone orchiectomy, Teronred was used at a dose of 1000 mg daily in combination with prednisone or low-dose prednisolone (10 mg daily).
Adverse reactions observed during clinical trials and post-marketing experience are listed in the table below by frequency category: very common (≥ 1/10); common (≥ 1/100, < 1/10); uncommon (≥ 1/1,000, < 1/100); rare (≥ 1/10,000, < 1/1,000); very rare (< 1/10,000) and not known (frequency cannot be estimated from the available data).
Within each frequency grouping, adverse reactions are presented in order of decreasing seriousness.
Table
| Organ systems | Adverse reactions |
| Infections and infestations | very common: urinary tract infection common: sepsis |
| From the endocrine system | uncommon: adrenal dysfunction |
| Metabolism and digestion | very common: hypokalemia common: hypertriglyceridemia |
| From the heart | common: heart failure*, angina pectoris, atrial fibrillation, tachycardia uncommon: other arrhythmias |
| From the vascular system | very common: arterial hypertension |
| Respiratory system | Rare: allergic alveolitis |
| Gastrointestinal system | very common: diarrhea common: dyspepsia |
| Hepatobiliary system | very common: increased alanine aminotransferase and/or aspartate aminotransferaseb rare: fulminant hepatitis, acute hepatic failure |
| Skin and subcutaneous tissue disorders | common: rash |
| Musculoskeletal and connective tissue disorders | uncommon: myopathy, rhabdomyolysis |
| From the urinary system | common: hematuria |
General disorders and injection site reactions | very common: peripheral oedema |
| Injury, poisoning and procedural complications | common: fractures** |